How well or how badly practitioners use their own bodies is critical to the length of time they will remain in practice. It also sets, whether consciously or unconsciously, a clear example for the patient of the concepts taught in this chapter. The treatment room environment is therefore not only a working environment but also a teaching environment and rightfully the first focus in this discussion.
The self-use element in bodywork remains a constant cause for concern. Both of the authors of this text have had the privilege and opportunity to teach existing as well as prospective practitioners and, in doing so, have become aware of the influence of poor body mechanics on the well-being of students as well as practicing clinicians. Cautionary advice to students as to how to stand and bend and lift and apply pressure, etc., should be reinforced by sanctions if these features are not applied when they are being marked during skill assessment. At the University of Westminster, London, students on the bodywork undergraduate pathway are evaluated for their own body mechanics during all practical assessments and examinations, with marks from this aspect of the evaluation carrying equal weight to those allotted to the care taken in patient handling.
Problems as diverse as low back pain, neck and shoulder dysfunction, as well as repetitive stress conditions involving the hands and arms are common among practitioners and are largely preventable. Many such problems arise through inappropriately designed working surfaces, as well as the height of the treatment table, the positioning of the practitioner’s body in relation to the table, the application of pressure and movement and similar factors.
A good ‘rule of thumb’ remains that if the practitioner is uncomfortable, awkward or straining when applying the techniques taught in this text, there is either a predisposing dysfunctional condition in her own body (for which treatment should be sought) or else she is incorrectly applying the technique, which may be due to table height, hand or body position or other factors which place undue strain on the practitioner. The application of the techniques in this text should always be comfortable and non-straining for the practitioner (and, of course, for the patient).
Similarly, the practitioner attending continuing education classes should be constantly reassessed by the instructors for body usage. Practitioners who have left their student years far behind often forget the basics of self-protection, perhaps because of the pressure of too heavy a caseload and/or of inappropriate work positions (due to injury or lackadaisical attitude or to poorly adjusted table height) all of which may have led to poor habitual patterns of use.
Among the guidelines that bodywork students and practitioners should be taught relating to ‘posture’ and ‘acture’ (active posture) are the following.
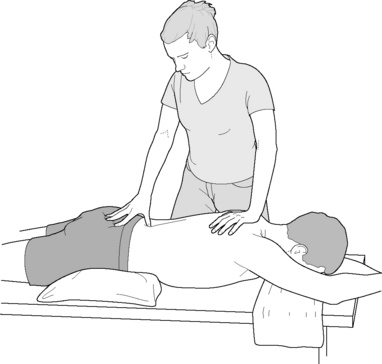
• Maintain a wide base of support. The feet should be separated with the potential for easy weight transfer from one foot to the other, allowing contact hand pressures to be increased or decreased as required by means of weight transfer rather than muscular effort (practice of tai chi encourages this type of movement). Balanced stance calls for careful positioning in relation to the treatment table and the patient, in order to be able to easily move the upper body and to transfer weight from one leg to another, without losing balance and without the need to readjust foot positioning. A wide base of support offers a chance for smooth movements without strain and creates a stable, centered stance which would not be easily perturbed by an unexpected need for alteration of position (Fig. 4.1).
• Maintain the spine in neutral as far as possible. This calls for flexion occurring (if possible) at the knees and hips and with the lumbar spine being required to produce only minimal flexion and extension movements during the application of treatment.
• Awareness of one’s own center of gravity, which lies just anterior to the second sacral segment (approximately 2 inches (5 cm) below the umbilicus and 2 inches (5 cm) deep), is important. Flexion of the knees and hips will encourage conscious movement of this center of gravity.
• The head and neck should be held in a ‘forward and upward’ mode, the typical Alexander technique model of posture in which there is a perpetual lengthening of the spine (from the head) rather than a slumping collapsed posture in which the weight of the head drags the upper body forward and down. During application of therapeutic measures any tendency for the upper cervical region to extend should be resisted, a particularly difficult habit for many to break (Fig. 4.2).
• Economy of effort relates to the concept of using the body efficiently in terms of reducing strain as well as energy output, thereby avoiding fatigue. Discussing the ‘principle of least effort’, chiropractor and Feldenkrais practitioner John Hannon (2000a) has described an example in which the standing practitioner engages the lateral border of the scapula of the sidelying patient in order to mobilize it.
The therapist positions himself so that his sternum faces the client’s scapular spine. He adjusts the table height until an easy folding of [his own] trunk is possible by forward bending at the hips (Fig. 4.3). His hands surround the top-most [superolateral aspect of the] scapula …By taking a broad, stable stance, it is possible for him to arrange his pelvis and trunk to counterpoise each other. In other words, by suitable arrangements, he creates an unstable equilibrium of his trunk upon his pelvis, and his legs upon his ankles…the therapist, by rocking his trunk forward upon his femoral heads, and by rocking his lower extremities backward upon his ankles, is able to maintain his balance [Fig. 4.4]. The reason for insisting upon a sense of balance is to avoid tensing of the fingers, stiffening of the arms, and holding of the breath, yet allowing the therapist to induce ‘therapeutic strain’ by merely tipping forward [and backward].
• Use of mechanical advantage encourages economy of effort and minimal personal strain for the practitioner. Hannon (2000b) uses the term ‘creating an irresistible force’ as he positions himself in relation to the patient and uses the forces available from gravity, inertia and skilled use of body mechanics and leverage to slowly and gently ‘oblige’ shortened or restricted tissues to yield, lengthen or mobilize. The difference, when attempting to stretch tissues, between use of ‘irresistible force’ and muscular force is the difference between gentle but persistent persuasion and coercion. Both ‘work’ but one is far more pleasant than the other.
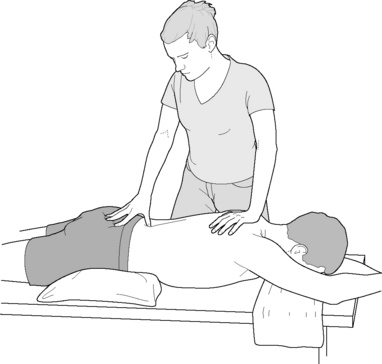
Figure 4.1 Practitioner’s posture should ensure a straight treating arm for ease of transmission of body weight, as well as leg positions which allow for the easy transfer of weight and center of gravity. These postures assist in reducing energy expenditure and ease spinal stress
(reproduced with permission from Chaitow (2010)).
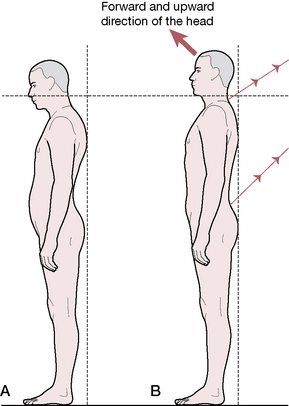
Figure 4.2 Diagram showing the preferred direction of movement in the typical Alexander posture, in which the head moves forward and up, while the lower neck and the lower back move backward and up.
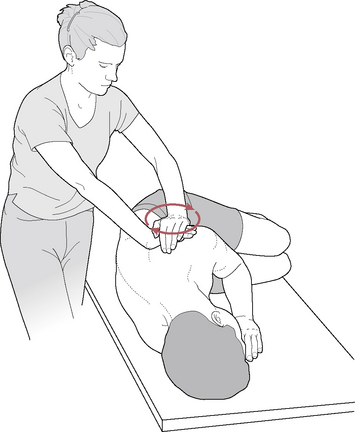
Figure 4.3 Application of therapeutic torque, achieved by careful weight transfer and positioning, as described in the text
(reproduced with permission from Journal of Bodywork and Movement Therapies 4(2): 119 with thanks to John Hannon DC).
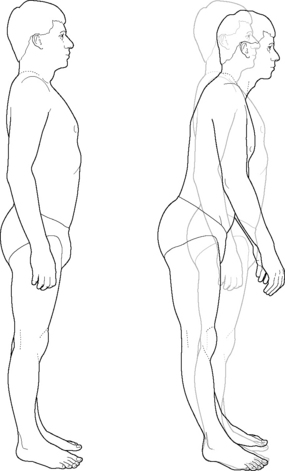
Figure 4.4 Demonstration of standing in ‘unstable equilibrium’ as described in the text
(reproduced with permission from Journal of Bodywork and Movement Therapies 4(2): 119 with thanks to John Hannon DC).
Quoting at some length from Hannon (2000d) offers the reader an opportunity to understand more fully the somewhat abstract terms ‘inertia, gravity and skilled use of body mechanics’. It is suggested that reference be made to the notes on tensegrity structures in Volume 1, Chapter 1 in order to appreciate the use of sound physics in the application of the forces Hannon describes. Particular note should be taken of the way Hannon describes practitioner positioning, since this is subsequently used to achieve the greatest possible mechanical advantage, with minimal effort or personal stress.
In the quotation that follows, part of the treatment of a hypermobile patient with chronic low back pain and muscle strength imbalance is described. Hannon carefully positions the patient in sidelying, using cushions, bolsters and wedges to achieve comfort, support and what he terms ‘repose’.
The therapist is sat on a stool, feet flat on the floor with the trunk hinged forward upon the sacrum. The ischia were perched solid, but freely rockable, upon the stool, with elbows wedged into the therapist’s distal medial thigh flesh. This allowed the bones of the thighs, elbows and spine to be stiffened into two triangles radiating out from the spine. [Fig. 4.5]…Gravity became the prime motive force for the treatment in this position; the practitioner simply rocked forward on the ischial contacts, and fell ever so slightly toward the client. Empirically, it seems that the client felt this touch to be much less strong and invasive as compared to that of clutched fingers pressed into the same point of anatomy. Rhythmic pressures were applied by a combination of trunk leaning and minimal [practitioner] thigh abduction/adduction. These movements drove the [practitioner’s] forearms forward into the contact with the client. The hands molded the contact upon the client’s thigh, remaining soft and malleable. … As the therapist rocked backward upon the stool, a tensile strain was applied to the client’s thigh. A twisting traction was created deep in the client’s thigh by selectively rocking and rotating upon one ischium and applying a compressive force strain with one hand and a tensile strain with the other.
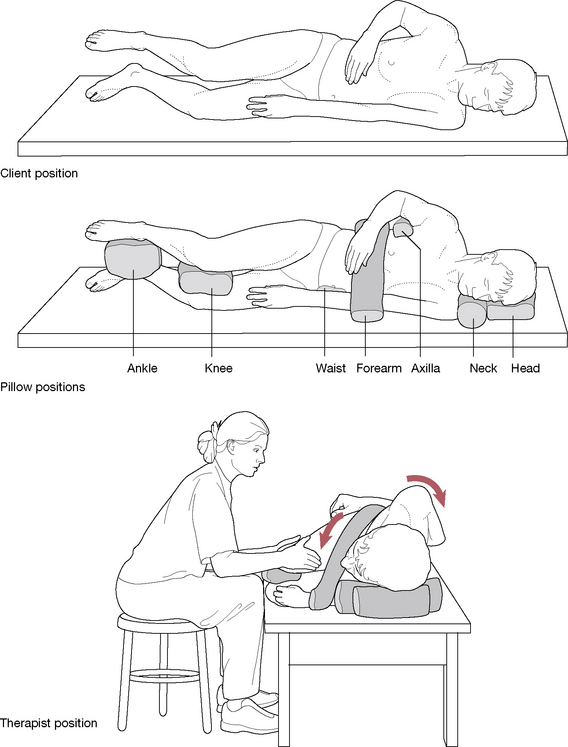
Figure 4.5 Therapist position to maximize stillness while performing myofascial release of the right proximal thigh (reproduced with permission from Journal of Bodywork and Movement Therapies 4(4):281 with thanks to John Hannon DC). Note: The authors have found that similar stable positioning of the patient is achievable using the bodyCushions™ available from Body Support Systems, Inc. Contact details are given below - on this page.*
These movements perfectly illustrate ‘least effort’ and utilize the transmission of forces through a tensegrity structure which has been created by the careful construction of an interaction between the practitioner and the client, in which any movement, whether pivoting on an ischial tuberosity or adduction of a thigh, transmits force through the contact hands and into the tissues. Hannon (2000d) then goes on to describe additional therapeutic processes in this case. The extensive extract quoted above gives insights into the use of forces such as gravity and inertia, which are freely available and which can be easily employed, without strain to practitioner or patient.
• A combination of the features of good ‘acture’ therefore involves sound positioning, a wide base of support, balance (and sometimes, in Hannon’s term, ‘unstable equilibrium’) and the ability to transfer weight and force by minimal repositioning of the practitioner’s body, employment of gravitational forces and tensegrity, all with the intent of achieving the principle of least effort (‘less is more’). A final thought from Hannon (2000c) is worthy of repetition. Stopping movement, but maintaining a monolithically static treatment contact would reduce some of the flow of sensation to the client and might sharpen their sensate focus. And stillness of the therapist would allow more control of the specific forces that impinge upon the client’s skin and joint fascial sensors. Just as an essential, if rarely considered, part of music is the silence between the notes, stillness may have a place in the manual therapist’s tool box. (see Box 4.1)
• It should be kept in mind that when the patient is placed in sidelying position, in most cases the height of the working surface changes. For example, the uppermost shoulder or hip is higher than the surface of the torso was when it was in a prone or supine position. It may be advantageous to keep a small platform nearby (such as is used in step aerobic classes) on which to stand, should elevation be needed in order to more effectively apply body weight. In the ideal practice setting, this problem could be eliminated by a hydraulic table, which could adjust the patient height with a touch of a button.
• For the patient’s comfort, bodyCushions™ may be used with the patient placed in various positions.* These cushions have been designed to encourage relaxation of the patient’s neuromusculoskeletal systems. It should be noted that the cushions add to the height of the working surface and the table height must be lowered, or the practitioner raised, in order to avoid strain.
Box 4.1 Hannon’s ‘treatment house-rules’ (Hannon 2000c)
These house-rules are guidelines for the practitioner for better self-use, based on principles derived from Feldenkrais concepts and clinical experience. The phraseology used by Hannon (on whose work these ‘house-rules’ are based) is non-technical and, hopefully, easily understood.
1. Sit whenever possible (‘why should the client get all the rest?’). Sitting provides stability.
2. Have your feet on the floor to ‘take advantage of the solid ground reaction force to aid in precise delivery of force’. This is not possible if seated with legs dangling or if standing with weight on one leg only!
3. Use rocking movements to apply treatment force. A solid sitting perch together with having both feet planted allows fine control of the forces involved in contact with the patient.
4. Use pelvic movement potentials. ‘By cultivating an erect spine, solid footing and toned abdominal and gluteal muscles’ the pelvis can be put to work in pivoting and translating movements which transfer to the forces applied to the patient via the relaxed contacts with the patient’s tissues.
5. With firm but gentle contacts it is possible, when seated, to introduce strain, torque and traction into the patient’s tissues, by rotating your pelvis, balancing yourself on one ischial tuberosity which acts as an axis and utilizing variations in pressure from one foot or the other. Hannon refers to this as ‘turning the other cheek’.
6. Position the sternum and spine to line up with the area being worked on to reduce unnecessary strain.
7. Have the forearms symmetrical and parallel to the lines of force involved in the handling of the tissues being treated. This releases rotational stresses in the arm and hand muscles.
8. Maintain hand contacts soft and molded to the tissues. ‘Your hands last longer that way.’
9. Avoid excessive effort as this ‘blunts your senses, coarsens your treatment, and clouds your day with fatigue’. It also creates stress in what Hannon calls your ‘clench zones’, including suboccipital region, eyes, tongue, jaw, throat and diaphragm (Fig. 4.6).
10. Breathe easily.
11. Keep elbows heavy and relaxed.
12. Keep the spine erect and easy, not stiff. The lumbar spine is more easily maintained in neutral if flexion takes place at the hip joints.
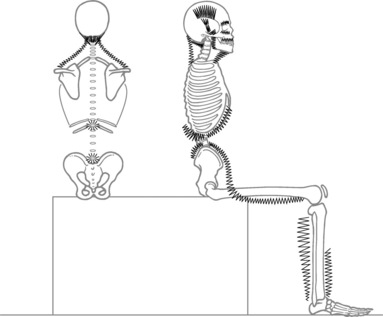
Figure 4.6 Common ‘clench’ zones when performing treatment in the sitting position. Notice the many areas of potential tension. To this list may be added those personally idiosyncratic areas of muscle activation
(reproduced with permission from Journal of Bodywork and Movement Therapies 4(4):270 with thanks to John Hannon DC).
Sitting in a car can be a health hazard, especially for the driver. The link between driving and back pain is well established (Wilson 1994). A man who spends half the working day driving is 300% more likely to develop a herniated disc than the non-driver. For heavy vehicle drivers, the risk rises by 500% (McIlwraith 1993).
Waddell (1998) has very strong opinions about the risks involved in sitting and driving, which he believes have more to do with the vibratory influences than the seated position. ‘Many studies show a higher prevalence of back pain, early degeneration of the spine and disc prolapse with driving. The key physical event seems to be exposure to whole-body vibration.’ He suggests that people who spend more than half their working time driving are particularly likely to suffer back trouble and points out that the vibratory frequency of many vehicles is 4–6 Hz which, according to Pope (1991), is also the resonating frequency of the spine. Wilson (1994) agrees that vibration and jarring increase the rate of muscle fatigue, accelerating the negative influence on discs of prolonged sitting. Good seating design together with good seated posture and optimal tire pressures, as well as the best possible automobile suspension, are all factors that can reduce the vibratory, jarring forces inherent in driving.
Some of the key elements involved in the production of back pain as a result of driving include the following.
• The design of the driver’s seat may be inappropriately offset in relation to the foot controls in some cars, causing a permanent torsion of one or both legs, or of the pelvis, when driving.
• The driver’s seat may not be adjustable for height, in which case the body size of the driver may be inappropriate for that particular car. There should be at least 10 cm (4 inches) head clearance when sitting comfortably, not slumped, and the shorter driver should be able to easily see over the dashboard without straining.
• The driver’s vision may be compromised due to the seating position and, if so, head, neck and back strain and distortion become likely. It is clearly easier for a short individual to increase height by means of a cushion than for a tall driver to contort to fit into a low-roofed vehicle. The height of the roof in relation to the height of the tall individual is therefore a more critical feature than the height of the dashboard is to a short person, since it cannot be as easily corrected. Some automobiles have adjustable seat height, which may eliminate this particular hazard.
• Seat design should ensure that the seat could be reclined and raised/lowered to meet the needs of the driver’s body type. Seating should also be contoured to support the back, ideally with an adjustable lumbar support area and side support.
• The headrest should be adjustable with a tilt potential.
• Lumbar support may be missing or non-adjustable. A lumbar roll or purchased car seat overlay which offers lumbar support can be added to those cars which lack adequate support.
• Poor steering-wheel design may create awkward body positioning, depending on the driver’s body type and other physical characteristics (for example, there may be special needs due to body height and/or length of the arms). Most such problems are eased if the steering mechanism is adjustable and further eased if there is power steering.
• Air conditioning, if used excessively and/or if streams of cold air are inappropriately directed, can exacerbate muscle discomfort and produce aggravation of trigger point activity, particularly in the neck and shoulder areas.
• The amount of time spent in the driving position, as well as the number of times the individual gets in and out of the car, are key contributing factors to the development of backache linked to driving. Within this text it is recommended to stop frequently to get out and move about; however, the effort of extracting oneself from the car can also be a stress factor and more so if the back is already irritated. Proper positioning of the body while getting in and out of the car is therefore a critical factor.
• Wilson (1994) lists the driving-related features, which were self-reported by a group of drivers with backache as aggravating factors:
1. sitting incorrectly 93% 2. reversing the car 50% 3. sitting in one position for too long 47% 4. getting in and out of the car 33% 5. operating foot pedals (clutch) 20% 6. inadequate lumbar support 10%.Solutions to all these problems are available, although sometimes at a considerable expense, including (at times) the need to purchase a newer, more appropriately designed vehicle. Other features that reduce driving stress include an automatic gear shift, power steering, cruise control so that the foot does not have to remain in an extended position, and quality suspension to reduce vibration factors.
Most driver-related problems, however, are solvable by inexpensive and relatively simple strategies such as inclusion of a lumbar support or a cushion to increase height, proper body usage when getting in and out of the car, the use of a small yet solidly based step stool when climbing in and out of high vehicles and by ensuring regular breaks if driving is prolonged, say 5–7 minutes every hour, for a stretch and a walk (Wilson 1994). Despite the obvious inconvenience, such breaks should be taken every hour, if possible, and not accumulated to be a longer break every 3 hours. This is especially important for the person who already suffers from back pain. Leisure time should include muscle-toning exercise activities that focus on the abdominal and back stabilizing muscles and should be incorporated into daily life and not just sporadically interspersed during a trip.
While seatbelts and airbags do indeed offer their own collection of possible injuries, as discussed in the following section, these injuries are potentially less harmful than those incurred if a serious motor vehicle accident (MVA) occurs without a restraining device. The following discussion addresses the potential injuries from these devices but it is not intended to imply that a better alternative would be to discard the use of the restraint or of airbags. Proper use of the restraint, better body and belt positioning, and the use of car seats for infants and booster seats for young children, have been shown to decrease the chances of serious injury or fatality and are wholeheartedly endorsed by the authors. Consideration of the injuries that may have resulted from the restraining devices, however, should be part of the assessment protocols for even minor MVAs.
Over and above its profound influence on seated posture, automobile design has the potential, through seatbelt and/or airbag-induced trauma, to contribute in a major way to injuries sustained in road accidents. Nordhoff (2000) offers clear insights into the processes that occur in relation to motor vehicle accidents. He also cites evidence that suggests that in many instances seatbelts are responsible for more injury than any other physical part of an automobile (although they undoubtedly reduce fatalities).
• Major research studies show that women report injuries from traffic accidents twice as frequently as men (Murphy 2000).
• A French study evaluated injuries in 1500 car occupants involved in motor vehicle accidents and reported that 47% of female occupants and 21% of male occupants had cervical injuries (Foret-Bruno 1991).
• A Swedish study showed that regardless of the size of the car involved, women incurred more neck injuries than men (Koch 1995).
• Nordhoff (2000) suggests this gender difference may be because of the smaller neck diameter in females, as well as (in general) smaller body mass and therefore a higher rebound velocity from seatbacks, especially with rear-end accidents.
Larder (1985) analyzed the pattern of symptoms following motor vehicle injury and found that:
• there was a mean patient reporting of 3.1 symptoms
• most common symptoms related to neck pain (94.2%), headaches (71.5%), shoulder pain (48.9%), low back pain (37.2%), visual disturbance (21.1%) and loss of balance (16.1%) along with other symptoms including vertigo, tinnitus and radicular irritation
• fatigue, anxiety, sleep disorders and a range of musculoskeletal problems, such as thoracic outlet and carpal tunnel syndromes, and TMJ disorders were also reported
• symptoms did not always appear soon after the injury, but often up to 96 hours later.
Chester (1991) noted that a diagnosis of fibromyalgia was present in more than 50% of 48 rear-end motor vehicle crash cases, in a 7 month – 7 year study.
A study involving over 100 patients with traumatic neck injury as well as approximately 60 patients with leg trauma evaluated the presence of severe pain (fibromyalgia syndrome) an average of 12 months post trauma (Buskila & Neumann 1997).
• The findings were that ‘almost all symptoms were significantly more prevalent or severe in the patients with neck injury [i.e. whiplash] … The fibromyalgia prevalence rate in the neck injury group was 13 times greater than the leg fracture group’.
• Pain threshold levels were significantly lower, tender point counts were higher and quality of life was worse in the neck injury patients as compared with leg injury subjects.
• Over 21% of the patients with neck injury (none of whom had chronic pain problems prior to the injury) developed fibromyalgia within 3.2 months of trauma as against only 1.7% of the leg fracture patients (not significantly different from the general population).
• The researchers make a particular point of noting that: ‘In spite of the injury or the presence of FMS, all patients were employed at the time of examination and that insurance claims were not associated with increased FMS symptoms or impaired functioning’.
Murphy (2000) reports that: ‘Post-traumatic FMS is usually unilateral in its presentation [because] most motor vehicle crashes load the human body with asymmetrical forces’.
Simons et al (1999) report that headache symptoms may not arise for weeks after the trauma, while Moles (1989) and Kaplan & Williams (1988) state that damage to the TMJ may not become apparent for months after the ‘whiplash’ has occurred.
The same [automobile accident] trauma that damages the musculo-skeletal system may cause similar injuries to other soft tissue, particularly the brain. The term mild traumatic brain injury [mild TBI] is used to describe subtle damage to the brain following trauma. Similar terms include post-concussion syndrome, and mild head injury. The word ‘mild’ is misleading, as the corresponding loss of function may be substantial or even disabling.
When someone suffers a cervical or temporomandibular strain following a whiplash-type injury, it is logical to suspect additional structural insult to nearby tissues. The same shearing forces that tear and damage the cervical musculature may also damage fascial structures and neurons in the brain and brainstem. The visual system is exceptionally vulnerable. Burke (1992) clearly correlates ocular motor complications with whiplash. Such damage can severely compromise the rest of the body through alterations in gait, as proprioceptive information reaching the brain becomes unreliable (see Chapter 3 on proprioceptive influences on gait).
A clear distinction is needed between the natures of injuries that are likely to be sustained because of front-end, rear-end and side collisions. Collisions that produce spin, such as seen with an oblique impact or when the vehicle is spinning prior to contact, can create complex patterns of trauma. Additionally, if the head and neck are rotated at impact, such as when the driver turns to look left or right for oncoming traffic, additional strain is applied to ligaments, annular fibers of the discs, myofascial tissues and joint surfaces, often with substantial consequences.
Other variables which determine the nature and severity of injury include seat positioning, occupant size, height, posture (both preexisting and that assumed at the time of impact), vehicle design as well as materials used (fiberglass, thickness of metal), vehicle interior design, size of vehicle, distance of occupant from interior features, presence of airbags, use or not of seatbelt, location and weight of objects within the vehicle that may become projectiles, as well as the speed and direction of impact.
In front-end collisions the driver can come into violent contact with interior structures including the steering system, knee bolster, windshield and floor. Depending on where they are located, passengers can come into violent contact with whatever is in front of them, which may include a front seat passenger or the driver, or receive impact from objects that lie behind them.
The driver or occupant, if wearing a seatbelt, is likely to sustain injuries at the seatbelt’s points of contact, most notably the neck. In a study of over 3000 accidents, 20% of occupants reported neck injuries (mostly minor) directly resulting from seatbelts, as against only 8% of unrestrained individuals (Morris & Thomas 1996).
A further study of almost 4000 accident occupants showed that 21% of the belted and 14% of the non-belted occupants reported neck injuries (Maag et al 1990) (Fig. 4.7).
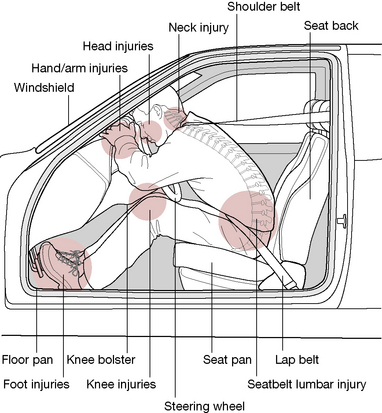
Figure 4.7 Frontal impact forces from interior elements of automobile in head-on crash
As Nordhoff (2000) explains: ‘With all restrained occupants, regardless of seating position, the seat belt is responsible for generating more injuries than any other contact source within the vehicle’. Most such injuries are minor and most occur because the seatbelt is working precisely as it was designed to do.
There are several reasons why seatbelts increase neck injury while reducing fatalities. First the three-point belts are designed with asymmetrical geometry, with one shoulder being restrained. Second the belts act as a fulcrum for energy to concentrate its loading on the occupant. With less of the human body to absorb energy, the neck takes the brunt of the forces. Third, submarining may occur in collisions in which the lap-belt is loose; that is, the occupant slides down the seat under the shoulder harness or lap belt.
In such circumstances severe damage may occur, including fatalities, as the vulnerable anterior neck takes the force of impact. This type of injury is more likely with small adults and children; the use of booster seats for children between 40–80 pounds is strongly urged (see Box 4.2).
Box 4.2 Protecting the child passenger
When a motor vehicle is involved in a crash, there are actually a series of collisions. When the vehicle collides with another object, the bodies of the passengers continue to move at the precrash speed. If a person is properly restrained, his body will impact against the restraining device (seatbelts or other restraint) very soon after the primary collision. If not restrained, the body will continue moving until it collides with the interior of the vehicle or with the ground or other object outside the vehicle. And, lastly, the internal organs will then impact against bony structures which enclose them (brain and skull, lungs and ribs, etc.), which can be mitigated somewhat by the degree of proper restraint by seatbelts, airbags and padding.
The objective in choosing and using restraining devices should be to reduce the chance of these impacts and, at the same time, reduce (as much as possible) potential injury by the restraining device itself by using it properly. Vehicle design, airbags and snug-fitting seatbelts (with shoulder harnesses) all assist in protecting the adult body during the crash. The tighter the seatbelts are adjusted, the lower the body’s overall deceleration, thereby reducing the potential rate of impact between the skeleton and internal organs (including the brain against the skull) (Weber 2000). Additionally, distributing the load of impact as widely as possible and onto the strongest body parts (in adults, primarily the shoulder and pelvis and secondly the chest) optimally reduces impact injury.
When being transported in motor vehicles, the immature bodies of children have special protective needs that change as the child’s body grows. In the early stages, before bones, ligaments and muscles offer enough support, rear-facing car seats help prevent cervical, head and spinal cord trauma. As the body matures sufficiently to better withstand the severe tensile forces associated with deceleration, forward-facing restraints can be employed. The type of restraint needs to be age appropriate and must be reevaluated as the childvs body matures. An adult seatbelt can be safely used without other restraining devices when five conditions are met simultaneously:
• child can sit with lumbar spine and upper buttocks fully against the seatback
• the knees bend at a 90° angle at the seat edge
• shoulder belt fits across the shoulder
• lap belt over the thighs or bony pelvis
• the child is mature enough to sit reasonably still during the ride (Sachs & Tombrello 2000).
Since the younger child (either backward or forward facing) is buckled into a restraining device by a harness or shield and then the child restraint device itself must also be buckled down, great care must be taken to assure that both systems are tightly fastened to avoid excessive movement or ejection of the child, or child with car seat, during a crash. Weber (2000) notes: ‘A large observation study in four states found that about 80% of child restraints were not being used as intended (Decina & Kneobel 1997)…Clearly a failure to anchor the CR [child restraint] or to harness the child is about the same as nonuse, but there are many other opportunities to do the wrong thing’. These mistakes may include inadequate tightening of the harness that holds the child, or of the seatbelt that restrains the car seat, or the use of the wrong type of seatbelt for that particular restraining device.
When the child matures to (about) 4 years old and 40 lbs and his height or weight surpasses the upper limits recommended by the manufacturer (many manufacturers use different weight and height limits so read instructions carefully), many adults erroneously conclude that the child should be advanced to adult seatbelts. At this stage, the child’s body is still too small to properly fit the adult belt. Proper placement of the seatbelt includes the lap portion of the belt fitting snugly across the bony portion of the pelvis and with the shoulder strap fitting across the mid-sternum and crossing the shoulder about halfway between the neck and the arm. With the child’s body (especially upon impact), the lap belt rides up into the fleshy abdomen and the shoulder strap onto the anterior cervical region, often resulting in serious (including spinal cord) injuries (Weber 2000). Equally or more dangerous is the practice of placing the shoulder portion behind the child or under the arm to avoid irritation to the neck, resulting (upon impact or even during hard braking) in the child submarining under the belt or being ejected over it, leading to serious injury or fatality. The child who cannot achieve a proper fit of both lap and shoulder belt should ride in a booster seat specifically designed to adapt the adult seatbelt to the child’s body.
A lap belt that is placed or rides up above the hips can intrude into the soft abdomen and rupture or lacerate internal organs (Rouhana 1993, Rutledge et al 1991). Moreover, in the absence of a shoulder restraint, a lap belt worn high can act as a fulcrum around which the lumbar spine flexes, possibly causing separation or fracture of the lumbar vertebrae in a severe crash…A belt-positioning booster (BPB) raises the child so that its body geometry is more like that of an adult and helps route a lap/shoulder belt to fit that body size.
The National Highway Traffic Safety Administration (NHTSA 2000) is responsible for developing a comprehensive 5-year strategic plan to reduce deaths and injuries caused by failure to use the appropriate booster seat in the 4–8-year-old age group. The NHTSA notes that in February 2000 they launched their ‘Don’t Skip a Step national booster seat campaign to educate parents about the risks of improperly positioned adult seat belts and the effectiveness of belt-positioning booster seats for children ages 4 to 8 years’.
The technology of restraining the occupants in motor vehicles (and particularly infants and children) is ever changing and advancing to improve the possibilities of survival of impact without serious injury or fatality. It is important that the latest information be accessed and passed on to the public (especially parents and caregivers) through health-care providers and educators. The following contact sources are provided to assist in this task. These websites are packed full of safety information regarding these as well as other safety issues.
• American Academy of Pediatrics – www.aap.org (great information for typical and atypical children)
• National Center for Injury Prevention – www.cdc.gov/injury/
• Insurance Institute of Highway Safety – www.highwaysafety.org
• National Highway Traffic Safety Administration – www.nhtsa.dot.gov
• University of Michigan Transportation Research Institute (UMTRI) Research Review (newsletter – $35/yr subscription) – www.umtri.umich.edu
Airbag injuries are different from those deriving from seatbelt restraints. There tend to be far fewer neck and skull injuries with airbags but far more brain injuries, as well as upper and lower limb injuries resulting from air-bag deployment. Caution has been suggested regarding the distance and positioning of the upper body and head of the driver from the steering wheel which houses the airbag. The force of deployment is significantly greater, as is the danger of head damage and facial laceration, when closer than 38 cm (15 inches) (Dischinger et al 1996).
Children under 12 years of age should not ride in a seat that has a frontal-impact airbag as serious injury and a substantially increased risk of fatality may result from the impact of the airbag. This is especially true for young children and, in particular, infants in rear-facing restraints placed in front seats with airbags. Regarding subsequent airbag deployment, Weber (2000) reports:
Accelerations measured at the heads of infant dummies in this situation range from 100 to 200 G, with only about 50 G considered tolerable for children represented by a 6-month size dummy. The rear seat remains the safest position for the pre-teen child, properly restrained in age/weight appropriate devices.
(Note: G = G force = accelerations or gravity produce this inertial force, expressed in gravitational units; one G is equal to the pull of gravity at the earth’s surface at sea level and 45° North latitude (32.1725 ft/sec 2 ; 980.621 cm/sec 2 ).)
Nordhoff (2000) describes the mechanisms of trauma relating to motor vehicle collisions.
• First mechanism: vertical (axial) lengthening of the spine – an ‘accordion’ effect created via seatback pressure.
• Second mechanism: segmental motion may occur beyond normal anatomical limits as sternocleidomastoid pulls on the skull when the torso moves forward and the head lags behind.
• Third mechanism: swift extension-flexion of the neck increases cerebrospinal fluid and blood pressure to approximately 10 times greater than normal for milliseconds (called the ‘blood hammer’), leading to damage to spinal nerve ganglia; injury to lower cervical and upper thoracic nerve roots and spinal ganglia due to mechanical strain during extension stress.
• Fourth mechanism: global hyperextension of the neck beyond the normal anatomical limits of its ligaments, joint capsules and muscles; even low speeds (under 10 mph) can produce musculoligamentous tears, hemorrhage and even disc avulsion, especially if the head was rotated at the time of impact. At higher velocities compression fractures of the vertebrae may result.
Side-impact collisions (Fig. 4.8) are commonly more severe than front-end collisions because there is little to absorb impact energy other than the side of the vehicle. This usually violently loads the occupant’s torso and pelvis laterally while the head remains behind. Cervical and back injuries commonly involve disc damage. Side-impact airbags are beginning to appear with industry efforts focused on development of side airbags that will minimize injury risk to occupants (Weber 2000).
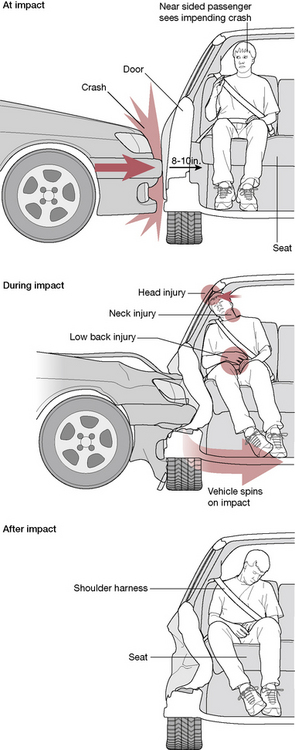
Figure 4.8 Occupant’s motion in a side crash
Several points made in Box 4.2 regarding children’s bodies apply also to those adults who are shorter than the ‘average’ body for which cars are designed. Additional details from that box remind us that, for the MVA patient, a series of collisions occurred, not just the primary one. After primary impact, the patient’s body (unless ejected from the vehicle) continues to move at the precrash speed until it is restrained by the seatbelts or other restraint, at which time the head/neck, arms, and legs continue to move until they reached the elastic limits of (or tore) their associated soft tissues, or impact the interior of the vehicle. The internal organs continue to move and very likely will impact against the bony structures that enclose them (brain to skull, lungs to ribs, etc.), each of these organs being enmeshed in an envelope of fascia that may also sustain injury or become an adherent ‘glue’ that fixates the organ to the bone. It is important when preparing a treatment plan to consider these and other possibilities, and to include assessment, treatment or referral to other health care practitioners in a whole body therapeutic approach.
Some of the challenges discussed with sitting in automobiles are also true on airplanes, while others faced in the airborne vehicle are unique. For instance, ‘taking a walk’ while in flight is a very brief, usually crowded experience, especially if encountering serving carts. Additionally, the frequent handling of carry-on luggage as well as check baggage can impose strains on posture, which must await the next ‘stop’ before adequate room for stretching, or movement is available.
The airline seat itself can impose structural stress on the posterior thigh (especially for those with short legs), lumbar region (where lumbar support is often inadequate) and on the cervical region (where seat design often does not fit appropriately, especially for the person who is not of average size). Although some newer models of planes offer adjustable lumbar support, optional footrest bars and other amenities that support body comfort, older model planes are still in service and offer little to adequately support the traveler’s frame.
Particular problems encountered in airline travel, as well as suggested solutions, include the following.
• Talking with the head turned to one side for an extensive time, which can activate trigger points in levator scapula (Simons et al 1999) and other cervical muscles. Active, repeated rotation to the opposite side periodically during the conversation to stretch the shortened muscles will help reduce risk.
• Falling asleep with the head in a tilted position can activate trigger points, especially with a cold draft blowing from the air conditioner (Simons et al 1999). An inflatable neck pillow can support the head while conscious effort to avoid drafts or cover the neck when sleeping will reduce risk.
• Prolonged sitting can shorten the soleus and gastrocnemius muscles, which can activate trigger points in them. The soleus pedal exercise (Fig. 4.9) can be incorporated while seated during flight for active stretch of the soleus as well as to enhance the vascular pumping action this muscle offers (Travell & Simons 1992).
• Trigger points may be activated in the hamstring muscles if these are compressed against the edge of the seat, especially if the legs are too short to comfortably contact the floor (Travell & Simons 1992). A briefcase, book or other carry-on items can support the feet to elevate the legs. Alternatively a small, portable folding footrest (which stores easily in carry-on luggage or briefcase) can be purchased from occupation therapy supply catalogs such as the one detailed below.* Non-folding versions are also available which can be placed at a desk, reading station or other areas where portability is not a consideration.
• A combination of dehydration, prolonged sitting (especially on long flights) and reduced oxygenation in pressurized cabins contributes to the risk of ‘economy class syndrome’, involving potentially life-threatening deep vein thrombosis (DVT)/pulmonary emboli. These conditions may occur from clots arising from pooling of blood in the feet and legs as well as cramped conditions. People most susceptible to this are those who drink too much alcohol, use sleeping pills and/or are overweight. Avoidance of alcohol, adequate water intake and movement of the limbs when seated are all helpful in reducing these risks.
• For anyone at particular risk of DVT (markedly overweight, history of venous problems especially previous DVT, congestive heart conditions, elevation of clotting factors postoperatively or postpartum, recent fracture resulting in elevated platelet coagulant factors) prophylaxis should also include the wearing of elastic support stockings during flight, as well as consulting (prior to flying) a medical practitioner to evaluate the possible benefits of anticoagulant medication prophylactically (e.g. mini-doses of heparin or warfarin (Tikoff 1983) or self-administered aspirin, or garlic extracts (Kiesewetter 1993, Phelps & Harris 1993)).
• People with breathing pattern disorders (such as hyperventilation) are put at extra risk on long flights where aircraft may reach 35 000 to 37 000 feet above sea level for 10–12 hours. Cabins are, of course, pressurized to prevent altitude hypoxia and to ensure the comfort of the traveler. While older aircraft (such as the Boeing 737) relied entirely on fresh air flowing through all the aircraft’s sections, fuel conservation strategies in modern planes have led to the recycling of used air, mixed with fresh air in varying proportions, which can result in the reduction of the levels of available oxygen.
• Hyperventilation is a classic manifestation of ‘fear of flying’ and those suffering this may experience signs and symptoms of hypocapnia (decreased arterial carbon dioxide tension). ‘Fear of flying’ courses may help and should cover these issues. Much of this training and conditioning is based on maintaining breathing control, as well as cognitive skills to manage fear (Bradley 1998).
• Concerns for air travel safety and security issues that create delays in the process of arriving at the plane produce anxiety, provoke adrenal responses and create additional stresses. Poor food choices within the airport and on the plane add to the body’s challenges to maintain adequate nutritional stores and healthy energy. Frequent travelers and business travelers, in particular, may resort to caffeine, ‘power bars’, and other substances, in order to maintain the energy needed to work during the flight, attend meetings upon arrival, and to complete the travel ‘mission’. Despite the body’s need for recovery from the trip, as well as from altitude and temperature variations and the impact of time zone differences, many often push through it, only to repeat the process in a few days (or hours) with the next leg of the journey.
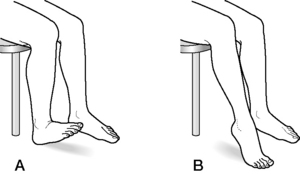
Figure 4.9 During prolonged seating, the soleus pedal exercise can enhance the vascular pumping action this muscle offers. The exercise is applied first to one leg then to the other, for 10–12 sets
(adapted with permission from Travell & Simons (1992)).
While society’s desire for ‘fashion consciousness’ drives the footwear industry’s design of shoes, the wearer’s demands for comfort, practicality and diversity of foot use also dictate strong needs. However, the basic reason that shoes are here to stay is that they protect the foot from the elements of nature. It is ironic that in attempting to prevent injury to the body’s contact with the ground, a vast collection of potential bodily dysfunctions has been created.
Since the foot brings man into immediate and direct physical contact with his environment, its constant exposure and susceptibility to injury more or less necessitates an artificial encasement, the shoe, which in itself can cause and compound many foot problems. Therefore, the judicious examination of the foot and ankle include the careful scrutiny of patients’ foot wear.
An extensive discussion of the ‘examination’ of the shoe (especially patterns of wear) is included in Chapter 14 while the following points are reviewed here for their implications to postural dysfunction, deriving from the close environment.
The reader is reminded that in the following discussion, the term ‘high heel’ includes not only the obvious ‘spike heel’ shoe but also ‘cowboy’ boots and less elevated ‘high heel’ shoes as well. The degree of elevation of the heel will certainly affect the degree of postural compensation needed, but lower levels of elevation can also be enough to cause pain and recurrent somatic dysfunction.
Braggins (2000) is succinct: ‘Shoes must be wide enough to allow all toes to function, otherwise postural balance cannot be maintained’. At the same time, the anterior transverse arch must be maintained and supported (especially if the heel is elevated) to prevent the development of splay foot. The importance of toe movement is further explored in Chapter 3 (Gait analysis) and in Chapter 14, which discusses the health and well-being of the feet and toes.
It is also important that shoes should hold the heel firmly so that a stable situation exists when the rear leg pushes off in the gait cycle. A loose shoe causes the foot to try to grip to maintain its position in the shoe and this changes the function of the whole leg. Schafer (1987) addresses the issue of how well the shoes fit.
The wearing of loose-fitting shoes encourages pronation. A well-fitted shoe should be constructed so that most of the weight is borne on the outside of the foot, which is supported by strong ligaments. The inside of the foot is supported by long thin muscles that easily fatigue and allow the arch to drop and the foot to pronate.
Mennel (1960,1964) had this to say about the wearing of high-heeled shoes.
In women accustomed to wearing shoes with too high a heel, the knees tend to be constantly flexed, the hips are constantly flexed, and the lumbar lordosis becomes exaggerated. There is a greater tendency for the involvement of the joints of the thoracic and cervical spines as well, because of an increase in the thoracic kyphosis and the cervical lordosis by compensating mechanisms. This disturbs their balance and prevents the maintenance of normal tonus in supporting muscles. This abnormal posture produces unfair wear and tear in their every joint, from the occiput to those of the toe digits.
Mennel is equally scathing about slippers that lack heels. ‘Shuffling in heelless slippers stretches all the soft tissues down the back of the leg, including the sciatic nerve (encouraging radiculitis), and throws a flattening strain on the lumbar lordosis.’
Braggins (2000) makes a more refined analysis of the effects of high heels, saying that the effect will vary depending on the degree of ankle mobility and the individual’s postural status. If there is a good range of plantarflexion, the feet might remain comfortable in high heels without undue stress on the low back, the altered stresses being absorbed in the foot and lower limb tissues. When plantarflexion is limited, however, Braggins suggests the knees will be unable to fully straighten when wearing high heels, causing the body to ‘tip forward with flexed knees and a flattened lordosis’ (Fig 4.10).

Figure 4.10 Footwear has a significant impact on the foot, the extreme of which is illustrated in the high-heeled shoe. Distortions of the foot will be reflected into the rest of the body with significant postural and structural implications.
Braggins’ perspective highlights the fact that identical stress factors (in this instance, the wearing of high heels) may have contrasting effects, depending upon the tissues being acted on. A supple musculoskeletal status of the foot, leg, pelvis and spine will tolerate the biomechanical insult that an altered position in space (created by high heels) imposes. A tight, less yielding musculoskeletal status, which is unable to absorb these same stresses as efficiently, is likely to result in the evolution of adaptational stress symptoms.
This difference in adaptational potential becomes an important topic for consideration when heel lifts and orthotics are being planned therapeutically While a leg length discrepancy, linked etiologically to a particular patient’s back condition, may seem to demand a heel lift to equalize leg length and so balance the sacral base, this may be inappropriate. Raising the heel could lead to increased symptoms or a whole new set of symptoms, possibly contralaterally, if the infrastructure on which the heel lift is acting is rigid and unable to absorb the necessary adaptive demands. Heel lift issues are dealt with more fully in Chapter 11.
Braggins (2000) suggests that there may be actual benefit in the wearing of high heels for individuals with shortened calf muscles while Kendall et al (1993) note that certain women with painful conditions of the longitudinal arch may benefit from wearing shoes with medium heel height. However, we urge the reader to fully consider alternative choices, which would be to examine for (and treat, when needed) trigger points and osseous misalignments, to strengthen hypotonic muscles and to use appropriate strategies to slowly lengthen the shortened muscles, rather than effectively cementing them into their dysfunctional state. Additionally, the temporary (and sometimes permanent) placement of an orthosis for correction of weakness of the arch or other foot pathologies may be beneficial (see Chapter 14).
Some of the changes resulting from the habitual wearing of high-heeled shoes are summarized by Schafer (1987).
As heel height is increased the center of gravity is moved posteriorly. When the calcaneus is elevated about half an inch [slightly more than 1 centimeter] above the base of the ball of the foot, its shaft is brought to a tangent with the Achilles’ tendon. …High heels, habitually worn, tend to shorten posterior and lateral compartment muscles and stretch the anterior [leg] muscles.
As the heels are elevated, weight bearing is moved more anteriorly on the plantar surface of the foot. With the use of a medium to high heel, the body weight is borne more on the metatarsal heads, which increases pressure on the tissues under the metatarsal heads, often resulting in the development of calluses, as well as placing stress on the transverse ligaments of this area, which can result in splay foot (loss of transverse arch). Kendall et al (1993) note that:
The effects of a fairly high heel can be offset, but only to a limited degree, by the use of metatarsal pads and by wearing shoes that help to counteract the tendency of the foot to slide forward toward the toe of the shoe.
When the foot slips forward within the elevated shoe, considerable deformation in toe position can occur, especially when toe width is crowded. Valgus position of the first metatarsal and the formation of bunions, hammer toe, claw toe and other acquired deformities resulting from inappropriate footwear choices and other stressors may affect general foot comfort as well as the gait (see Chapter 14 for more details on shoes and foot health).
Shoes with platform heels or wedged soles, which have little ability to flex, can create complex stresses involving the alterations they demand in the biomechanics of walking. The most obvious biomechanical necessity prevented by the inflexibility of this type of shoe is the need to flex the metatarsal heads during forefoot rocker (see Chapter 3), with much of the rest of walking movements being created by pelvic and hip action. Compensations for inability to flex the first MTP joint, in particular, as well as the other four digits can have substantial consequences as the knee, hip and lower back attempt to accommodate lack of normal foot function (see Chapter 3).
Thompson & Caughlin (1994) estimated that four particular procedures (bunionectomy, hammer toe repair, neuroma excision, bunionette correction), the cause of which they directly relate to high fashion footwear, accounted for approximately $1.5 billion operative corrections in the US in 1991. ‘When one considers that several other problems (soft corns, hard corns, claw toes, intractable plantar keratoses, sesamoid abnormalities, hallux rigidus and toenail problems) were excluded from this calculation, the estimated total cost resulting from the wearing of high-fashion footwear of $3 billion per year is undoubtedly a conservative one. Noting that frequency of foot problems are much greater in women and attributing this to the fashionable footwear that so many feel compelled to wear, they conclude, ‘Changing societal footwear habits requires an awareness of the dangers of and damage done by ill fitting, tight shoes. …Increased public awareness is the most important preventitive step … in decreasing the huge expenditure of health care dollars for these forefoot problems.’
Butler (1991) suggests that the wearing of high-heeled shoes places the peroneal nerves under increased tension and that tight shoes can add to the problems resulting from this. A further etiological feature of neural entrapment or irritation involves the manner in which particular shoe design can exert pressure on susceptible neural and circulatory structures. A common open-toe shoe design involves straps that apply pressure onto the anterior tarsal tunnel and the tendon of extensor hallucis brevis, both of which are ‘anatomically vulnerable’ sites for the deep peroneal nerve. Butler explains:
Kopell and Thompson (1963) identified an entrapment neuropathy of the deep peroneal nerve under the inferior extensor retinaculum. MacKinnon and Dellon (1988) reported an additional site of entrapment as being distal to the anterior tarsal tunnel, overlying the junction of the first and second cuneiforms with the metatarsals. Here, the medial (sensory) branch is crossed by the extensor hallucis brevis. MacKinnon and Dellon identified an aetiological factor as being the straps from a particular design in women’s shoes. This could be regarded as a form of external double crush.
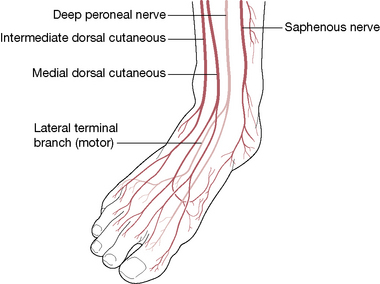
Figure 4.11 Saphenous and peroneal nerves in the foot
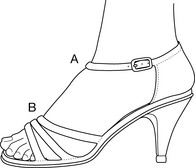
Figure 4.12 A common design of women’s shoes places the straps over two anatomically vulnerable sites for the deep peroneal nerve. In A the nerve is in the anterior tarsal tunnel and in B the nerve is under the tendon of extensor hallucis brevis
Orthos in Greek means ‘straight’ or ‘correct’; orthotics is the science concerned with the making and fitting of an orthopedic appliance which corrects or makes straight, and an orthosis is the appliance itself. While the term ‘orthotics’ is commonly used to refer to the appliance, this text will employ the above usages when discussing these appliances.
The objective of a foot orthosis is to create a correct configuration of the foot once it has lost its natural ability to sustain that status. There exist a variety of orthoses that support arches, joints and other areas of the foot (Prior 1999).
• As a rule orthoses are placed inside the shoe and may be relatively soft or fairly rigid, depending on the needs of the situation.
• Some orthoses are semi-molded, such as those found in good running shoes, and others are custom made to meet the specific needs of the individual.
• Some preformed orthoses are made from materials (such as ethylene vinyl acetate) that can be modified when heated with a hot air gun (by a qualified podiatrist) to fit precisely the shape of the foot. Additional fine tuning can then be achieved by use of wedges to produce control of the dysfunctional pattern for which the orthosis is being created.
• Variable factors which determine the type of orthosis used, and the material from which it is constructed, include economics, the weight of the individual, the precise problem being addressed, the activity involved (walking, standing, running, etc.), as well as the type and style of shoe.
Overuse patterns have been associated with the use of mobile/cell phones for SMS messaging.
One study evaluated a variety of postural and functional features associated with use of mobile/cell phones, and with short message service (SMS) messaging (Gustafsson et al 2009). Fifty-six young adults (15 healthy and 41 with musculoskeletal symptoms) were assessed for differences in regard to gender, as well as between individuals with, and without, musculoskeletal symptoms.
The findings of this study can be summarized as follows:
• There were significant gender differences in muscular activity in the extensor digitorum and the abductor pollicis longus during SMS messaging, with females having higher muscle activity levels than males. The reasons for this appear to relate to smaller hand size in females requiring greater abduction.
• Females tended to have fewer pauses between key applications than males.
• Individuals with symptoms tended to move their thumbs with higher speed, compared to those without symptoms.
• Unsurprisingly perhaps, trapezius muscle activity was consistently higher in subjects with symptoms, though not to a statistically significant degree.
• In contrast, there were significant differences in muscle activity in the abductor pollicis longus (APL) between subjects with and without symptoms, with subjects without symptoms having higher levels of muscle activity.
• While there is as yet no adequate explanation for this apparently contradictory finding, it seems that the lower muscle activity in the APL, in the group with symptoms, is similar to findings in a different study, that identified lower EMG activity in extensor carpi ulnaris, in high activity phases of low precision computer mouse work, during experimental muscle pain (Birch et al 2000). (italics added)
• Those subjects with symptoms tended to have fewer and shorter pauses compared with those without symptoms.
• Relative to sitting, entering an SMS while standing increased trapezius muscle activity.
• Females, when compared to males, typically had higher muscle activity levels and they tended to work in greater thumb abduction, to move their thumbs with higher velocities and to have fewer pauses in the thumb movements.
• Subjects with musculoskeletal symptoms had lower muscle activity levels in the abductor pollicis longus and tended to move their thumbs with higher velocities and to have fewer pauses in the thumb movements compared to those without symptoms.
• Different studies have demonstrated that, during computer mouse use, females tend to have higher muscular activity levels than males (Karlqvist et al 1999, Wahlstrom et al 2000).
• Fontana et al (2007) showed that occupations involving repetitive thumb movements, with too few rest breaks, are risk factors for osteoarthritis of the thumb.
• Excessive SMS texting is a key feature in patho-physiology of the first carpometacarpal joint arthritis (Ming et al 2006).
The design of clothing and jewelry, like shoes, is driven by the consumer’s personal taste and is not always considerate of what is best for the health of the body. Elastic restrictions of lymphatic flow (Singer & Grismaijer 1995) as well as continuous compression of myofascial tissues could lead to localized edema and to local energy crisis consistent with that seen in the formation of trigger points (Simons et al 1999). Consideration should be given to restricting items, such as watchstraps worn around the wrist, elastic and tight waistbands on pants and skirts and the elastic components of foundation garments (bras, girdles).
Chronic clothing constriction (CCC) (Singer & Grismaijer 1995) can have a long-term effect on the tissues. The following list includes some of the most obvious examples of constrictive clothing and of postural strain associated with the use of accessories. The reader is encouraged to consider other possibilities of chronic pressure placed on myofascial tissues by apparel and accessories.
• Tight shirt collars and ties can induce trigger point referral patterns in the SCM (Simons et al 1999) or can reduce blood flow to the brain, especially in people who have arteriosclerosis (Singer & Grismaijer 1995).
• Knee-high stockings or socks with elastic bands to restrain them can perpetuate trigger points in peroneus longus, extensor digitorum longus and gastrocnemius (Travell & Simons 1992), can restrict lymphatic flow and contribute to the development of varicose veins (Singer & Grismaijer 1995).
• A heavy coat, the shoulder strap of a purse or the straps of a bra can activate upper trapezius trigger points (Simons et al 1999).
• Heavy necklaces can pull the head and neck forward, placing undue stress on posterior cervical muscles (personal and clinical experience of author JD).
• Gripping the mouthpiece of a pipe or cigarette holder between the teeth or wearing an ill-fitting denture can activate trigger points in the masseter muscles (Simons et al 1999).
• Straining head postures can occur associated with contact lenses or new spectacles to avoid light reflections in the lenses or to look through the appropriate portion of the lens (Lockett 1999, Simons et al 1999), thereby affecting posterior cervical muscles, jaw and postural muscles.
• Walking with a cane that is too long or not used properly can activate trigger points in the upper shoulder area (Simons et al 1999).
• The use of a walking frame, especially when improperly held too far in front of the person, can induce forward head position which can, in turn, activate trigger points in cervical and masticatory muscles.
• Elastic bands worn at the upper arm area (such as in the cuff of a short sleeve) can irritate deltoid, biceps and triceps and restrict lymph flow, the avoidance of which is especially important with post-mastectomy care.
• A wallet worn in a back trouser pocket can irritate gluteal muscles and piriformis and can cause ‘back-pocket sciatica’ (Travell & Simons 1992) which can often be relieved by a ‘walletectomy’ and inactivation of the trigger points.
• The chronic use of a back brace can weaken spinal support muscles, making them especially vulnerable when demand is placed upon them when the back brace is not being used. Limiting the duration of time spent in the brace as well as the addition of exercises to strengthen the lower back and abdominal muscles may prove to be a better choice than constant use of the brace.
• The use of a heavy backpack, purse or luggage strap can strain the trapezius (Simons et al 1999) and/or anterior shoulder muscles. The use of heavy backpacks is now seen frequently in even young children to whom lockers are no longer available in schools and who are transporting heavy books which are sometimes close to their body weight, both from class to class and between school and home.
• The strain of carrying a child, either on the hip or on the shoulders, produces postural strain not only from the increased weight being borne but also from the distortions being applied to the human frame. Women tend to carry a child on a laterally thrust hip (thereby distorting the pelvis and lumbar areas as well as the weight-bearing points of the legs and feet) while men tend to carry a child atop the shoulders (thereby pressing the head and neck into a forward thrust position). Additionally, since the kinetic bundle being carried is seldom still, the adult’s body must also constantly adjust to postural repositioning based on a dynamically (and often abruptly) changing center of gravity.
• Many devices which have been designed to help carry the infant child (cloth slings, back and front packs, basket-type totes) offer their own assortment of postural strains, including forward head positioning, occlusion of upper trapezius by strapping mechanisms or the strain of carrying the additional weight (of the child plus the carrying device) by one arm.
• Pressure on the rib cage from a tight bra can activate trigger points in serratus anterior, latissimus dorsi or serratus posterior inferior (Simons et al 1999).
• The rigid underwire of a bra can irritate fibers of the right pectoralis major or intercostal tissue between the 5th and 6th ribs, which can form and provoke cardiac arrhythmia trigger points which can disturb the heart’s normal rhythm (Simons et al 1999).
Singer & Grismaijer (1995) have discussed at length the constrictive nature of brassieres and the possibilities of suppression of normal lymph drainage of the breast area. They note:
Affecting lymph vessels more than blood vessels, minimal pressure on the body can cause lymph vessels to close while leaving open the arteries, capillaries, and veins. This means that blood continues to flow to the constricted area, feeding it oxygen and keeping the tissue alive, but that the tissue develops a buildup of lymph fluid surrounding the cells.
As surrounding fluid accumulates, nourishment and waste removal can be inhibited. This reduces all cellular functions. Toxins accumulate, poisoning cells even further. Ultimately, long-term starvation of the tissues and accumulation of toxins can lead to degeneration.
They note higher risk of breast cancer in those women who wear bras for more than 12 hours per day and that ‘a woman who wears her bra twenty-four hours a day has a 125-fold greater chance of developing breast cancer than does a woman who does not wear a bra at all.
The choice not to wear a bra may not be one that is physically or socially comfortable. However, the choice to reduce wearing time, to loosen the degree of restriction or to change to another type of support when at home (such as a bathing suit or leotard) which may be less occluding of lymphatic flow is suggested as an alternative to constant restriction. Additionally, periodic lymph drainage therapy of the breast, chest and arms is suggested for those who have a more constant use of constrictive clothing or who present symptoms consistent with the conditions mentioned.
Lewit (1983) is very specific in his condemnation of some forms of undergarments for some physical types.
A suitable brassiere is extremely important for women with heavy breasts. All too often we see women patients lifting their breasts with brassieres that are too small, with narrow straps that cut deep into the flesh of the shoulders. That constant drag on the shoulders is enough to foil any attempt to treat the cervical spine or to correct body statics.
More robust support systems are strongly advocated in such circumstances by Lewit. Simons et al (1999) suggest wider, non-elastic bra straps or distributing pressure by placing a soft plastic shield under the strap.
Observation of static sitting is revealing, as is observation of the individual as he goes through the motions of sitting down and rising from a seated position. When seated, a number of evaluations should be made, ideally after the individual has had a chance to relax and assume his comfortable seated posture.
• Is the individual sitting squarely on both ischial tuberosities or more on one side than the other?
• Are the legs crossed? If not, the question should be asked as to whether crossed-leg sitting is the norm for this individual and if so, which leg is most likely to cross the other (see Chapter 11 for discussion of the value to sacroiliac stability of cross-legged sitting).
• Has a slumped sitting position been assumed?
• What are the individual’s hands and arms doing? Are the arms folded across the chest or are the hands resting on the lap, on the thighs or some other variation?
• When chairs have armrests, do the person’s arms rest comfortably on them or does use of the armrest require the person to lean to one side in order to contact the resting surface? When the upper arm (humerus) is shorter than normal, which is apparent when the elbows do not reach the level of the iliac crest when standing, the person tends to lean to one side (straining quadratus lumborum and the lateral cervical region) or to lean forward onto both elbows (straining the posterior cervical and paraspinal muscles) (Travell & Simons 1992). When armrests are set too high, the shoulders will elevate, thereby shortening the upper trapezius.
• If sitting at a desk or table, is the person leaning onto the surface for support? Ideally, the surface should be at a height that, by letting the upper arm hang naturally, the elbows could be rested on the surface while sitting erect (i.e. without bending forward) and without bearing body weight on the forearms or elbows.
• Are the feet both touching the floor, supporting the weight of the legs, or are the legs tucked under the chair, or stretched in front of it, or perhaps even one or both legs folded directly under the person’s hips and being sat upon (i.e. foot in direct contact with the thigh or hip)?
• If the feet do not touch the floor, is the person slouching in order to reach the floor? If so, a foot support (preferably one with a slanted surface) should be provided.
• If the feet are on the floor, what is the angle of the thighs to the floor: parallel, sloping downward so that the hip is higher than the knee or are the knees higher than the hips? Much will depend on relative leg length and chair size/height.
• Is the back of the chair being utilized for support? And if so, is it used correctly or being slumped against?
• When viewed from behind in a seated position, are the iliac crests level and the spine straight? When functional scoliosis and unlevel pelvis are noted in a seated position, this could be due to a small hemipelvis. Travell & Simons (1992, Chapter 4) discuss examination and correction for this skeletal anomaly, which they note is more likely to be presented in a person with lower leg length inequality.
• It is always useful to ask the individual to demonstrate his usual work position, especially if this involves sitting. A ‘candid camera’ photograph taken by a co-worker when the person is least expecting it (and brought to the examination) may reveal habits of use of which the person is completely unaware, especially near the end of a long work session or when the person is fatigued.
• If at all possible, it is also extremely useful to examine his car seat for its suitability (Lewit 1983). The condition of the seams of the seats, and the springs or stuffing inside the seat, will greatly influence the support of the pelvis and can be a factor in allowing a unilateral pelvic drop, especially if the person is in the car frequently and/or for long durations. This is also true of the favorite overstuffed chair or recliner.
Galen Cranz (2000a), who is both a professor of architecture and a qualified Alexander trainer, has focused attention on the common chair as a particularly dangerous piece of equipment that is capable of exerting major influences on posture and biomechanical health.
The right angle seated posture usually rotates the pelvis backward, flattens the lumbar curve, and throws the entire spine into one large C-shape. In order to see, a person’s eyes will remain horizontal, so while the spine changes, the position of the head does not, which means that the joint between the two is distorted. Specifically, all the cervical vertebrae extend forward, while the weight of the head comes back and down, rather than forward and up, in relation to the neck. The problems that flow from this pattern include back ache, neck ache, problems with vocal production, eye strain, sciatica, shallow breathing. (See Fig. 4.13)
The ideal seated position involves the creation of a relationship between thigh and spine of approximately 135°. This ‘ideal’ angle is achieved in perching on a high stool or in using the Norwegian-designed ‘Balans’ chair, in which weight is rested on the shins. A disadvantage of this kneeling position is that the feet lose the opportunity to provide proprioceptive feedback.
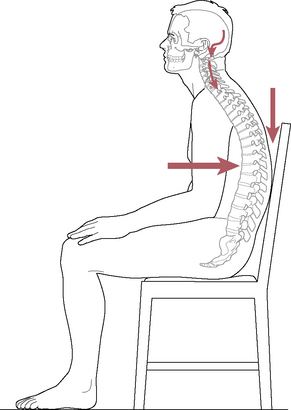
Figure 4.13 The right angle seated posture encourages slumping and in order to see while slumped, the head rotates back in relation to the top vertebrae, exerting a downward pressure on the spine. This slumped position prevents normal respiration, as well as creating multiple stresses in muscles and joints
(reproduced with permission from Journal of Bodywork and Movement Therapies 4(2):92, original drawing by Don Jacot).
Where standard seating is used, Cranz (2000b) suggests the following criteria be observed as far as possible.
• The ideal height of the seat should be 5 cm (2 inches) less than the height of the top of the individual’s knee from the floor.
• The seat should tilt forward to assist in creating the open angle between spine and thigh.
• A tilted seat that is 10–15 cm (4–6 inches) higher than the ‘ideal height’ suggested above (for sitting) would create a perching chair.
• The seat of the chair should be flat, non-contoured and firm with no more than between 1 and 2.5 cm (maximum 1 inch) thickness of upholstery.
• The seatback should be flat with a gap between the seat and the backrest to allow space for buttocks.
• There should be armrests (see also Box 4.3).
Box 4.3 Assessment of seated posture
Ideally, the individual should be assessed in the working and home environment in order to evaluate sitting posture, especially for deskwork, using computer and/or typewriter, and relaxing/leisure settings. The following criteria should be met when sitting for any length of time, i.e. more than a few minutes in a work context (see separate notes on postural considerations for musicians) (Fig. 4.16).
1. When seated at a desk/table with shoulders relaxed (i.e. not hunched or rounded) and elbows flexed to 90°, the forearms should be approximately 5 cm (2 inches) from the work surface so that the keyboard thickness allows keying with minimal stress to wrists, elbows and shoulders.
2. The chair height should be adjustable and (ideally) able to swivel.
3. The feet should be able to rest flat on the floor or on a slightly sloping surface directly below the knees, which are flexed to 90°. The feet are not curled under the chair, as would be the case if the chair/work surface height is too low, or unable to reach the floor if the chair is too high.
4. The hips and knees should be at approximately the same height when sitting comfortably or the knees should be a few degrees lower than the hips if the sitting position is on a seat that slopes slightly forward.
5. A slanted footstool, angled toward the sitter to approximately 10°, should be used if the feet cannot comfortably be supported by the floor (see p. 96 for details to order footrests).
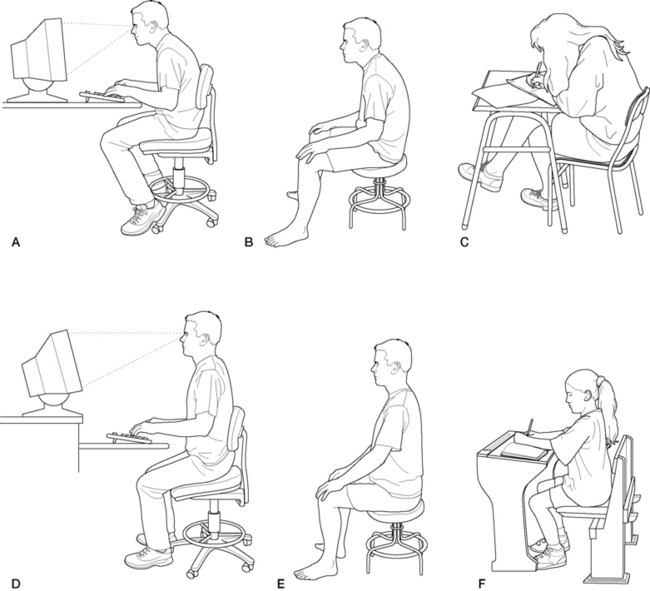
Figure 4.16 A: Inappropriate seated position for computer work forces head forward and stresses spine. B: Slumped seated position where weight is taken on sacrum. C: Writing at a flat table of inappropriate height encourages distorted posture. D: Balanced sitting at a work station. E: Balanced stool sitting, on ischial tuberosities. F: Balanced seating at ‘old-fashioned’ school desk.
6. The chair should be on castors for ease of movement (with built-in friction or chair mat if used on uncarpeted floor).
7. The chair should be stable with a wide base of support and therefore not be able to tilt or tip back or to the side on that base when body weight is transferred (however, the chair back may have a tilt safely built into it).
8. The seat of the chair should be able to tilt forward between 5° and 10°, which encourages improved posture for the lumbar spine and pelvis. If not, a wedge-shaped cushion could be used to achieve this.
The front edge of the seat should be rounded to avoid undue pressure on the posterior thigh (waterfall design).
The seat should be covered with high-density foam and well upholstered with a material that does not allow for build-up of heat (i.e. something other than vinyl or leather).
If the chair is a recliner, its back should be able to tilt to approximately 30° from the vertical and be capable of being fixed in that position rather than being supported by springs.
There should be ample leg room under the work surface, with a suggested depth of not less than 55 cm (22 inches) and width of 70 cm (28 inches) (Wilson 1994).
The work surface should be slanted for writing and reading tasks (or the materials being worked on or read should be slanted using a copy holder or other adjustable surface) and angled from 15° to 30°.
Lighting should be carefully arranged to avoid glare and should be adequate to ensure easy focusing on what is being observed.
Keyboards should be separate from the computer screen if one is being used.
A wrist support should be used if at all possible when keying or typing for any length of time.
The (ideally contoured) chair-back should support the normal curve of the lumbar spine and should therefore be adjustable for height and pivot, to take account of the particular body shape and needs of the individual.
The chair arms (if present) should be adjustable for height (or removable).
Regular breaks should be taken from seated work (a few minutes every 30 minutes is ideal) to stand and stretch and move around.
Brugger’s relief position exercise should be applied every hour or so in the seated position (see Box 4.4).
Lee (1999) highlights one of the key problems relating to sitting – the chair.
The average chair appears to be designed for the 5ft 10in (178 cm) man. Individuals less than this height must slide forward in the chair if the feet are to reach the ground. This motion places the line of gravity behind the ischial tuberosities, thus encouraging flexion of the lumbar vertebral column and the pelvic girdle (i.e. slouching [with loss of normal lumbar lordosis]). Individuals greater than this height have more difficulty controlling the optimal posture of the upper girdle [when seated]. To reach the desktop, they must lower the trunk, thereby flexing the cervicothoracic portions of the vertebral column.
• The feet should be flat on the floor.
• Legs should be uncrossed.
• Knee joints should be lower than hip joints.
• Pelvis should not be rotated posteriorly.
• The spine should retain its normal curves.
• The chest should appear open and not crowded.
• The head should be balanced on the neck rather than tilted backward.
• The eyes should be able to look at work, objects or people within a 15° zone without strain.
• While sitting, the patient should be observed for balance from the front as to levelness of pelvis, shoulders and ears.
• A lateral view should indicate the relative positions of the head and shoulders.
• Alexander technique looks beyond the posture during sitting and takes a great interest in how the individual gets into and out of the seated position. Indeed, anyone who has experienced lessons in Alexander technique will be familiar with the repetition of the sitting and standing process, as reeducation of correct usage slowly begins.
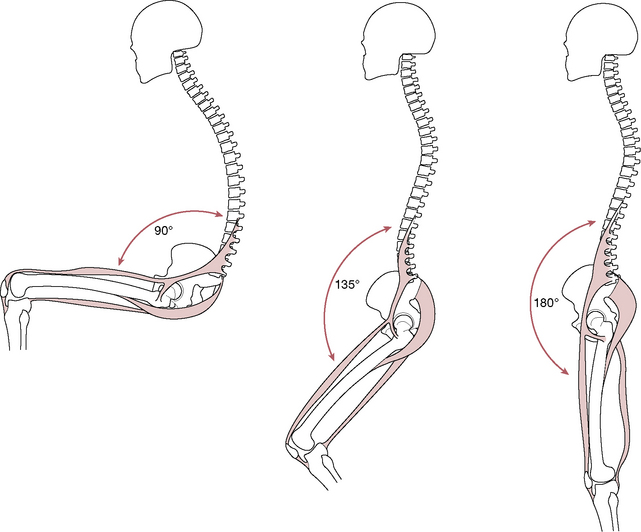
Figure 4.14 Note the spinal contours in the perched seated position (B), halfway between sitting (A) and standing (C), in which the lumbar curve is retained automatically
(reproduced with permission from Journal of Bodywork and Movement Therapies 4(3):157, original drawing by Denise Hall).
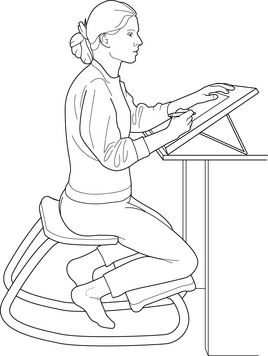
Figure 4.15 The original Norwegian kneeling chair, designed by Opsvik, provides an angle of approximately 135° between spine and thigh, retains the lumbar curve and allows much of the weight to rest on the shins
(after Journal of Bodywork and Movement Therapies 4(3):162).
Barlow (1975) discusses the act of sitting, from an Alexander technique perspective.
What should happen is that – with the heels apart from each other and the toes turned out – the kneecap should move continuously forward over the line of the foot, pointing approximately between the big toe and second toe. As the knees move forward the body will begin to descend. At this point most people will:
• pull their heads back
• throw the lower chest forward
• throw the pelvis backwards.
Barlow suggests that instead of this (as in Figure 4.17), the body should descend between two vertical lines as in Figure 4.18. ‘The pelvis should not push back and the lower chest should not push forward. Depending upon the height of the chair, the vertical axis of the body can then move backwards in space.’
Figure 4.17 Most people pull their head back, push the chest forward and pelvis backward, as they sit onto a chair
(after Barlow (1975), with permission).
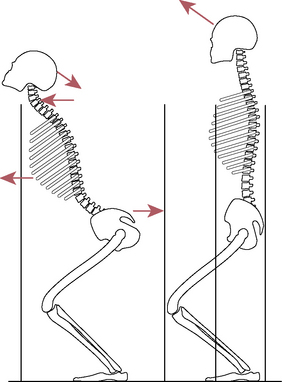
Figure 4.18 Instead of the position shown in Fig. 4.17, descent should be balanced and should allow the individual to stop and return to upright at any time. Barlow says: ‘The knee should move continuously forward over the line of the foot, and as the knee moves forward the body descends’
(after Barlow (1975), with permission).
It is at this point, Barlow asserts, that most people ‘fall’ backward into the seated position. He insists that this will not occur if the head is not retracted (‘tightened back’) during the act of sitting, but is instead directed forward at the top of the neck. The reader is invited to test this personally at this juncture, by placing a hand on the base of the skull to span the suboccipital musculature and to first stand up from sitting and to then sit down again, while noting the almost automatic (habitual) tendency to ‘chin-poke’ at the commencement of each of these activities and to be in virtual ‘free-fall’ by the time the buttocks meet the chair surface. Changing this habit so that sitting becomes a balanced and controlled activity, with the neck remaining open and lengthened, is one of the cornerstones of Alexander technique retraining. It can take months for this to take place without conscious thought. The benefits in reduced neck and spinal strain, reduced energy wastage and enhanced general function have to be experienced to be believed.
Despite this commendation of Alexander rehabilitation methods, caution is necessary. As Dommerholt (2000) points out:
In general, assessment and treatment of individual muscles must precede restoration of normal posture and normal patterns of movement. Claims that muscle imbalances would dissolve, following lessons in the Alexander technique are not substantiated in the scientific literature (Rosenthal 1987). Instead muscle imbalances must be corrected through very specific strengthening and flexibility exercises, since generic exercise programs tend to perpetuate the compensatory muscle patterns. Myofascial trigger points must be inactivated using either invasive or non-invasive treatment techniques. Associated joint dysfunction, especially of the cervical and thoracic spine, must be corrected with joint mobilizations. Once the musculoskeletal conditions for ‘good posture’ have been met, postural retraining (Alexander or other methods) can proceed.
We are in complete agreement with Dommerholt’s perspective, which is very much in line with that adopted throughout this volume. It is one in which undesirable maintaining factors are seen to require therapeutic input, through applied and self-applied interventions (stretching, toning, etc.), so that balance and mobility are restored prior to the introduction of reeducational programs.
There is outright disagreement between experts as to how much harm comes to the spine through inappropriate sitting postures. There is, however, a reasonable consensus as to the stress imposed on the spine as a whole, which can aggravate existing dysfunction. There is general agreement that poor sitting results in muscular strain, as well as head/neck strain (Fig. 4.19).
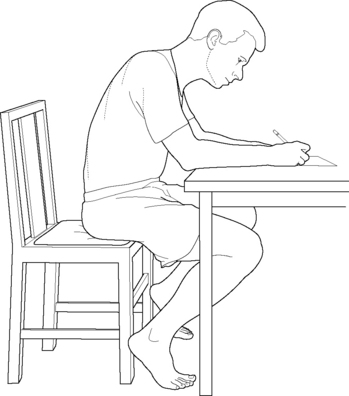
Figure 4.19 Poor sitting habits as a common cause of spinal problems
(reproduced with permission from Journal of Bodywork and Movement Therapies 3(3):147).
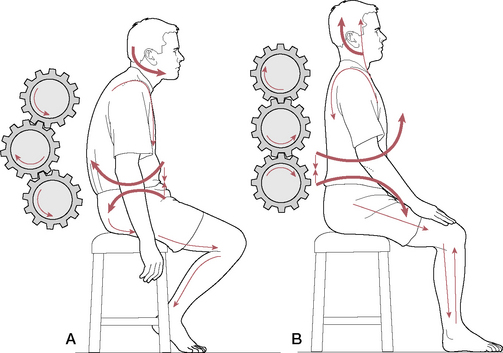
Figure 4.20 Seated postural stresses are demonstrated graphically by means of cog-wheels which suggest the lines of force operating during poor and balanced sitting
(reproduced with permission from Journal of Bodywork and Movement Therapies 3(3):148).
McKenzie (1981) is clear in his view that: ‘Almost all low-back pain is aggravated and perpetuated, if not caused, by poor sitting postures in both sedentary and manual workers’.
Waddell (1998) disagrees with the idea that sitting can actually cause back pain. He cites Bigos et al (1998) whose review of the literature found ‘no acceptable scientific studies on the effect of sitting’. He does, however, acknowledge that sitting in one position may aggravate already existent back pain.
Waddell argues: ‘Disc pressure in L3 is greater when sitting compared with standing, but this is static loading and the pressure is very low compared with that required to cause experimental damage. There is no other bio-mechanical evidence that sitting may damage the spine’.
Heffner (2000) strongly supports the concept of poor sitting habits as a common cause of spinal problems (contradicting Waddell).
Poor sitting postures are the most common cause for failure of the articular supportive structures in the spinal column. They, therefore, become the number one predisposing factor in the development of mechanical disorders for the back and neck. Poor sitting postures lead to protruded head carriage and are a commonly reported cause of neck pain. Static loading in faulty sitting or lying postures will lead eventually to problems within the cervical spine. (italics added)
A special problem is posed [in sitting] by prevention of head and neck anteflexion. Because the plane of the visual field must correspond with the plane of the object we are looking at, inclination of that object is what matters. If the book we are reading or the paper on which we are writing lies on a horizontal desk, raising or lowering the desk will not prevent us having to bend the head or neck forward. What is needed is a tilted surface.
People who habitually sit with the lumbar area stretched (flexed) constantly place abnormal tension upon the weak posterior aspect of the anuli and the soft tissues and facets of the posterior motion units. In addition, habitual sitting in lumbar flexion leads to a loss of the range of motion of lumbar extension, which influences segmental motions in sitting, standing and gait.
Liebenson (1999) has offered a chiropractic perspective of the damage done in poor sitting (Fig. 4.20).
The upright posture is dependent on the interaction of the three spinal curves. The lordotic cervical, kyphotic thoracic, and lordotic lumbar curves. When an individual sits the lumbar spine (commonly) becomes kyphotic, the thoracic kyphosis increases even up to the lower cervical spine, and the cervical cranial junction hyperextends. Anteriorly the sternum and symphysis pubis become approximated, compressing the diaphragm. The correction [offered by the Brugger relief position, see Box 4.4] separates the sternum and symphysis [pubis], and restores normal spinal curves.
Box 4.4 Brugger’s relief position exercise
Lewit (1999) and Liebenson (1999) point to the work of Brugger (1960) who has devised a simple postural exercise known as the ‘relief position’ which achieves a reduction of the kyphotic posture which often results from poor sitting and so eases the stresses which contribute to neck and back pain (Fig. 4.21). Instructions are as follows.
• Sit at the edge of the chair, perching on the end.
• Place feet directly below the knees and then separate them slightly and turn them slightly outward, comfortably.
• Roll the pelvis slightly forward to lightly arch the low back.
• Ease the sternum forward and upward slightly.
• Rotate the arms outwards so that the palms face forward.
• Separate the fingers so that the thumbs face backward slightly.
• Draw the chin in slightly.
• Remain in this posture as you breathe slowly and deeply into the abdomen.
• Repeat the breathing 3–4 times.
• Repeat the process several times each hour if you are sedentary.
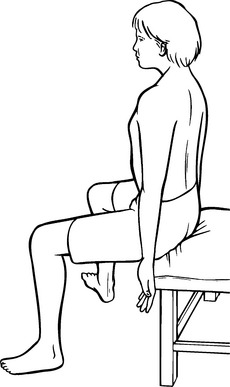
Figure 4.21 Brugger’s relief position, as described in the text
(reproduced with permission from Journal of Bodywork and Movement Therapies 3(3):149).
We believe that while Waddell’s view may be correct as to the link between sitting and low back pain being more one of aggravation rather than being necessarily causal, the evidence suggested by Cranz (see above) and others, relating to a general whole-body strain resulting from poor sitting, is beyond doubt. Harm to spinal structures deriving from poor sitting habits, therefore, may relate less to the positions adopted than to the amount of time spent in these positions. Waddell acknowledges a time-related influence in his observation regarding the dangers of the driving position, although he adds another factor, that being car vibration (see p. 91).
A factor that seems to go unremarked by most observers relates to the effect of slumped driving postures on respiratory function. The thoracic excursion required for normal breathing is frankly impossible when slumped, something that becomes instantly obvious when applying the Brugger relief position (see Box 4.4).
In recent years, the use of computers has moved explosively into all areas of life. From the library to the grocery store, from writing textbooks to learning how to read and even within the performing arts, computer usage now permeates many tasks which less than a decade ago involved little or no digital technology. The computer brings information and ideas previously not easily available directly into the average home, tempting the inhabitants to spend more and more time statically confined in repetitively strained positions for hours on end. Not only are the average hours spent at the computer increasing, usage is starting at an earlier age, with numerous programs available specifically designed for the toddler and preschooler.
Ricky Lockett (1999) views computer usage as a potential cumulative trauma disorder (CTD) in his extensive text on computer use and its effects on the body. He notes that while computer work enhances mental stimulation, the price one pays for it is loss of physical activity.
Children today are interacting with computers rather than engaging in physical play. As a result, they are the fattest and most unfit kids in American history. These conditions may predispose them to more heart disease and degenerative processes such as arthritis. There may be even more severe consequences when inactivity is forced on a growing, maturing and changing body.
Unless steps are taken to properly position the body while using the computer, to take frequent breaks and to stretch and recondition the muscles strained by excessive computer use, numerous musculoskeletal complaints and conditions may emerge. Listed among the many conditions Lockett associates with computer usage, office work and other sedentary tasks are thoracic outlet syndrome, carpal tunnel syndrome, cubital and ulnar tunnel syndromes, De Quervain’s tenosynovitis, epicondylitis, bursitis/tendinitis of the elbow, shoulder or wrist, tension neck syndrome, TMJ disorders, myofascial trigger points, plantar fasciitis, backache, headache, fatigue and eye-strain. ‘The accumulation of insults is what pushes the structure over the edge: from typical aches and pains to persisting, sometimes incapacitating pain.’
Elsewhere, Lockett notes:
Research has also demonstrated that multiple insults result in inflammation, swelling and edema, and this accumulation of insults causes the cumulative trauma disorders. Those conditions are the result of micro-injuries to the tissues. Part of the healing phase in the body’s attempt to heal micro-injuries involves an increase in fibrous production, characterized by the introduction of scar tissue. Without proper stress, the scar tissue lies down in an unorganized fashion and may, in fact, become the problem. (See Volume 1, Chapter 1.)
Research has not yet concluded the effects of other potential dangers associated with prolonged exposure to computers, such as the effects of radiation, noise pollution or mental/emotional stress.
Since it is apparent that computers, the Internet and the associated hazards (known and unknown) of computing are rapidly becoming part of everyday life for a vast number of people, it is more important than ever to understand the concepts presented in this text for application to repetitive stress and cumulative stress disorders. Stretching, strengthening and self-treatment should be part of the daily preparation for (as well as recovery from) computer stress. Lockett concludes:
It boils down to these factors: how well you take care of your body; how well you listen to those aches and pains; your company culture in regard to work demand and rest; effectiveness of early intervention approaches; and commitment by employer and employee to preventing cumulative trauma disorders…Through exercise your body becomes more resilient and is able to handle more of the stressors the world has to offer. In essence, exercise is medicine.
Note: Particular attention should be paid to the information contained in Box 4.3 insofar as it describes ideal conditions for desk and, by implication, computer work.
Sleep patterns are easily disturbed by a variety of factors ranging from emotional distress to pain as well as disturbances to normal life rhythms. Recovery of a normal sleep pattern is extremely important for many reasons, including the fact that much of the body’s tissue repair process takes place during sleep, when growth hormone is released by the pituitary gland (in stage 4 sleep).
Braggins (2000) observes: ‘There are no rules about the correct way to lie…but any pillow support used for pain relief should be discarded as soon as possible to restore freedom [to move]’. When pain or dysfunction exists, it is important to help the patient to find comfortable repose positions which can assist in obtaining adequate sleep as well as avoiding aggravating dysfunctional conditions which are trying to heal. However, it is also important that long-term use of supports does not create its own collection of distortions.
Lewit (1985) distinguishes between the sleep position advice that is given to patients with a cervical or a low back problem. He points out that many neck problems and headaches are worse in the morning after sleep and that it is critical to ensure the right degree and type of neck support during sleep. What is advised, however, depends on the patient’s habitual position of repose. ‘It is best to let the patient demonstrate his favoured sleeping position, and then to determine the height of support.’ This will vary depending on whether the individual lies squarely on the side, partially rotated, with shoulder forward or back or whether (against all advice) he sleeps prone. In the case of someone who sleeps prone, a habit usually deriving from childhood, ‘the most suitable compromise for those who cannot drop this habit is to place a pillow under the shoulder on the side to which the head is turned, thus lessening head and neck rotation’.
Lewit continues: ‘If symptoms are mainly in the low back we need to know whether the patient (habitually) lies on his side, supine or prone. If the answer is supine or prone, and symptoms occur during the night, or if the patient is wakeful, the trouble is usually due to lordosis’.
The advice Lewit offers includes asking the patient to try to avoid either supine or prone sleeping positions and to choose sidelying instead. If the patient insists on sleeping supine a pillow should be placed under the legs to induce relaxed hip flexion. If prone sleeping is insisted on, despite strong advice to the contrary, a cushion beneath the pelvis will reduce lumbar lordosis.
If sidelying sleeping induces discomfort, a scoliosis may be involved and a cushion beneath the waist should be used to support and straighten the lumbar and lower thoracic spine. Sidelying posture also requires support of the uppermost leg to avoid rotation of the pelvis and the resulting strain on the lumbar spine. Unsupported sidelying posture can result in irritation of the quadratus lumborum and activation of trigger points within this muscle (Travell & Simons 1992). This is also true of sidelying positions on the treatment table (Fig. 4.22).
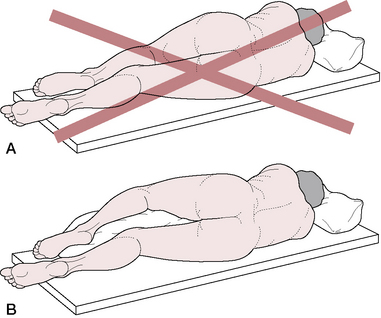
Figure 4.22 A: Poor sleeping postures can produce strain in lower back, hip, shoulder and neck musculature, resulting in activation of trigger points as well as structural consequences. B: Appropriate positioning with pillows reduces postural strain, shown here for lower back and hip region
(adapted with permission from Travell & Simons (1992)).
The artful use of pillows, bolsters, cushions and wedges can make all the difference between comfort and discomfort and, therefore, between sleep and insomnia. These principles may also be applied to sidelying positions used in the treatment room, which will enhance relaxation of tense tissues.
The simplest first step should be to encourage sidelying posture for sleep, with a cushion(s) between the side of the head and the sleeping surface, which allows the head and neck to remain parallel with the sleeping surface (not sideflexed). One absolute prohibition should relate to solid foam pillows, which have a tendency to resume their original position, so failing to accommodate to head and neck requirements for support. A variety of cervical support pillows, involving different shapes, contours and degrees of softness, are available. A trial-and error approach to finding what is best suited to the individual is called for, as there is certainly no universal ‘one size fits all’ solution to identifying what will be appropriate in a given case.
When sidelying, a cushion can be placed between the flexed knees or thighs to reduce pelvic rotation, side flexion or torsion. While some people are certainly comfortable when putting the cushion between the knees, if the legs remain straight this does not necessarily offer stability to the pelvis, which may then rely upon muscular tension of the torso for that stability. In such a case, a cushion placed under the uppermost (flexed) thigh and knee (the lower leg remaining straight) will reduce pelvic rotation and torsion while decreasing stressful tension on the lateral hip tissues. Travell & Simons (1992) note while addressing trigger points in the gluteus medius muscle: ‘The best sleeping position may be half-supine, that is, turned halfway between lying on the unaffected side and on the back, with the torso supported by a pillow’.
The relative firmness or softness of the sleeping surface is also a matter of individual taste. Prescribing a hard surface (‘orthopedic mattress’) used to be medically fashionable but it is now known that too firm a surface is unyielding, unsupportive of body contours, uncomfortable and unacceptable (Braggins 2000). As long as the sleeping surface offers reasonable support and is not uneven or sagging, a relatively firm bed with a softer sleeping surface is the logical choice (Fig. 4.23).
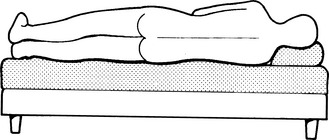
Figure 4.23 Sidelying sleeping position on a firm bed which has a soft surface maintains the spine in a supported position
Braggins notes that waterbeds provide an even distribution of support, which becomes increasingly important for anyone spending long periods in bed due to illness or disability. A waterbed heater should be used to maintain a fairly constant (warm) water temperature to avoid even mild hypothermia, which could result in activation of trigger points when the body tissues become chilled by too cool water.
Hannon (1999) discusses tactics for achievement of a restful position for the patient who is to receive bodywork by ‘supplying the client with a compelling surface on which to relax’. The same guidelines, somewhat simplified, apply to achieving a comfortable sleep position for anyone who is in pain. Adapting Hannon’s ‘patient positioning’ to a sleep situation is best done by illustration rather than written description, as shown in Figures 4.24-4.27.

Figure 4.24 On the side, pillow may be placed between the knees and lower legs such that the muscles of the thigh are relaxed and the lower extremities are approximately parallel although flexed at the knee. This prop placement is well tolerated for long periods of time; many people (pregnant women, those with hip arthritis, wasting of the thigh muscles) will prefer to use pillows such as this while sleeping on their sides
(reproduced with permission from Journal of Bodywork and Movement Therapies 3(1):61).

Figure 4.25 In this sidelying position the forearm is placed such that the middle of the forearm is balanced on the fulcrum created by the mid-axillary line of the rib cage. This allows the muscles of the shoulder girdle, specifically the brachialis, biceps, triceps and rotator cuff muscles, to be relaxed along with the latissimus dorsi and the serratus anterior. Often this allows deeper lateral excursion of the breath which further relaxes the shoulder muscles. Use this position only for a few minutes at a time since many people have slight shoulder instability combined with muscle imbalance. This often leads to asymmetric loading of the involved joints, which may tug at the pressure-sensitive layers of the affected joint capsules
(reproduced with permission from Journal of Bodywork and Movement Therapies 3(1):61).

Figure 4.26 A large pillow may be suggested to people with lower back pain. The person is arranged to allow the arms and legs to be supported and with the limbs parallel to each other. Often a lower back release and a deeper abdominal breath will be obtained. This effect is maximized if the patient is instructed to notice the moment the belly pushes into the girth of the pillow while simply breathing normally. The mental effort of self-observation will distract the patient long enough for this novel, for most people, position to act on the excess muscle activity
(reproduced with permission from Journal of Bodywork and Movement Therapies 3(1):62).
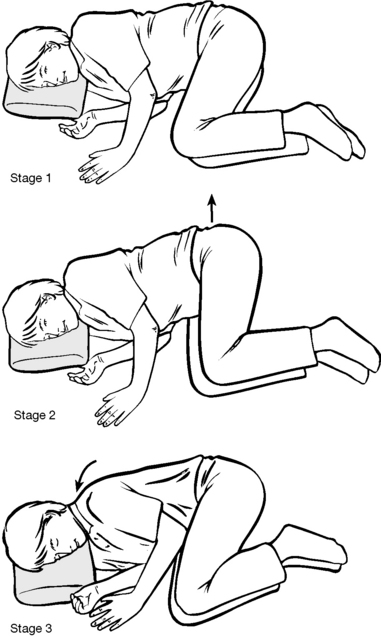
Figure 4.27 A fetal curve may be useful in obtaining deeper breathing and relaxed deep spinal intrinsic muscles along the length of the spine. The procedure is completed in three stages. In the first stage the patient is instructed to flex into a fetal curve. Minimal flexion at both the junctions of the neck to the trunk and the spine to the pelvis is often noted. Second stage involves passively pulling on the belt so the spine is placed into a greater kyphosis with the apex at a lower thoracic spine. The last stage is to bring the entire upper body into more flexion. As a unit, the head and shoulders are pulled into a fully tucked and comfortable position. This position is usually tolerable for long periods of time. If the person resists being placed into this position, either by active muscle activity or through the passive lack of elongation of the fascia and ligaments, respect the reluctance and only apply this fetal curve to a minor extent. The great value of accurately observing breath changes allows a practitioner to adapt the posture or prop for greatest effect. Too much stretch will provoke stiffness and/or pain, sometimes delayed. Too little stretch fails to encourage repose. In either case, an experienced observer will adjust the extent of the posture or prop’s effect to quickly bring about a relaxed breath, knowing that muscular repose will follow
(reproduced with permission from Journal of Bodywork and Movement Therapies 3(1):62).
Film of an individual taken during restful sleep shows a remarkable degree of activity as the sleeping position is modified 2–3 times per hour. This alteration of position is important to prevent the pooling of blood and to avoid sustained compression on supporting tissues. One of the key stimuli that cause a change of position relates to remarkable reflexes, involving nasal function (see also Box 4.5).
Box 4.5 Sleep, nasal breathing and backache
Nasal breathing is a part of normal function during sleep. Air passing to the lungs via the nose is humidified, warmed and cleansed. As it passes across the protective nasal mucosa with its forest of cilia and network of lymphatics, arteries and veins toward the lungs, air is monitored by extremely sensitive neural receptors. Barelli (1994) summarizes:
The autonomic nervous system and anatomic control of the nasal mucosa provide, when contacted by bacteria or by chemical stimuli, reflex cholinergic responses which influence the beat and secretions of the mucosa through ciliary activity.
It has been demonstrated that there exist nasal reflexes with many parts of the brain and spinal cord, connecting to practically all structures supplied by the cranial and cervical nerves (Mitchell 1964). Barelli cites proven reflex nasal connections to the ears, throat, larynx, heart, lungs, diaphragm, abdominal organs and the peripheral blood supply. Cottle (1980) showed that unilateral nasal narrowing or blockage can decrease diaphragm excursion on the same side by as much as 5 cm (2 inches).
This brief summary of often forgotten nasal influences impacts on the subjects of sleep positioning and backache in a somewhat surprising manner. Barelli (1994) points out that nasal function directly affects body positioning as follows.
• When lying on the side the turbinates of the lower nostril become congested and the nasal lumen closes.
• This leads to unilateral breathing during sleep.
• After a period of time movement of the head is initiated to trigger a turning of the body, so ensuring the alternate nostril’s opportunity to function. ‘A poorly functioning nose may allow the body and head to remain in one position and can cause symptoms such as backache, numbness, cramps and circulatory deficits’ (Davies et al 1989). And not surprisingly, if there is nasal dysfunction, sleep dysfunction may follow.
• Barelli concludes apocalyptically: ‘The quality of sleep, the quality of breathing, and the quality of life can all depend on adequate nasal function’.
Among the factors that might negatively impact on nasal function are biochemical features such as infection, allergy and/or intolerances (to inhaled or ingested substances). Sensitivity to environmental substances will be aggravated by higher than usual levels of circulating histamine which itself can result from disturbed breathing patterns (such as hyperventilation) which can arise from emotional causes, including anxiety (Timmons 1994).
Biochemical obstructions involving the ethmoid, vomer or other nasal structures may also result in nasal dysfunction and all that eventuates from it. Since secretions might be modified in target areas associated with active trigger points (Simons et al 1999), any triggers lying in the temporalis, masseter or sternocleidomastoid muscles (for example) might effectively alter nasal congestion status, with profound influences, as Barelli indicates.
These thoughts help to reinforce the conceptual and practical interrelationships between biomechanical, biochemical and emotional factors in illness causation and health promotion, which are discussed more fully in Volume 1.
A further thought, which emerges from this brief nasal focus, is that biochemical influences, deriving from aromatic substances, might offer profound therapeutic benefits for sound physiological reasons, as aromatherapists have long claimed.
Kapandji (2000) guides us to the appropriate way of investigating biomechanical problems in the musician. ‘In addition to the usual static and dynamic stresses applied on the whole spine, additional stresses are applied when playing instruments that depend on the playing position and the nature of the instrument being played.’
In other words, account needs to be taken of the relative postural distortions involved in violin, guitar and piano playing (as examples) as well as the idiosyncratic characteristics of the individual and the amount of time spent in the playing position (including practice and rehearsal time).
Kapandji highlights the key differences between those who play symmetrically (drummers, light wind instrument players such as clarinet, oboe, etc.), asymmetrically (violinists, guitarists, wind instruments held to one side, such as French horn, saxophone, flute, etc.) and while walking (members of brass bands, for example). Within the framework of the postural demands of a particular instrument, a range of variations exists. For example, a piano player may sit appropriately, with the height of the stool, the distance from the instrument and the body size and shape of the player all coordinating to produce minimal stress. However, some piano players adopt a hunched and rounded upper body posture, with the player’s face closely approximating the keyboard, while other players lean back and have outstretched arms, where ‘their pelvis is tilted posteriorly, the lumbar curvature is straightened and the thoracic is increased, as in a kyphosis that is the result of age’ (Kapandji 2000) (Fig. 4.28).
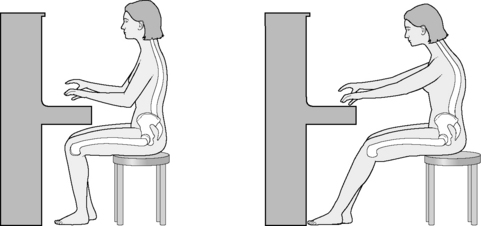
Figure 4.28 Postural stress in relation to piano playing
Where asymmetry is built into the playing of an instrument, as in the guitar, the risks of additional stress patterns emerging are greater. In the right-handed guitar player, the left shoulder is pulled down and the right upward, while the pelvis is tilted down on the right to accommodate this, creating a marked scoliosis (Fig. 4.29).
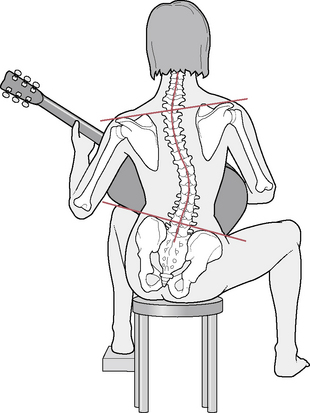
Figure 4.29 Postural stress in relation to guitar playing
Though influential, static positioning is not all there is to playing an instrument. Dommerholt (2000) points out:
Musical performance is probably the most complex of motor tasks combining artistic creativity, emotional expression and musical interpretation with a remarkable level of sensory motor control, dexterity, precision, muscular endurance, speed, and stress of performance.
He goes on to discuss just how much influence ‘body postures and movement patterns’ have on the resulting performance. He tells us that: ‘Musicians are usually not aware of any postural deficits, although postural misalignments, especially forward head postures, are very common’.
Any resulting dysfunction and pain can significantly interfere with the ability of a great many musicians to perform optimally. Dommerholt (2000) makes an important statement, citing Buytendijk (1964), when he suggests that a purely biomechanical approach to dysfunction relating to the playing of musical instruments is inadequate. ‘Musicians express their musical dialogue partly through their body postures and specific movements, which can be considered their innermost emotional expression.’ Indeed, it is also suggested that the movement and physical attitude of the player may correspond to the musical score and may play an esthetic role in the performance. Significantly, then, the static position of the player may be misleading diagnostically and only viewing an active performance would allow a full understanding of what stresses are involved and whether one set of stresses may be counterbalanced by another. As Dommerholt points out: ‘By moving through the entire functional range of motion [the musician] can avoid extreme static postures and possibly improve the musical interpretation’.
• Facial pain is reported to be prevalent among violinists, violists and brass players (Taddey 1992). Dommerholt (2000) reports successful treatment of severe facial pain in a violinist, by deactivating digastric muscle trigger points.
• Meador (1989) has reported myofascial latissimus dorsi and teres major trigger point involvement as contributing to a viola player’s symptoms.
• Dommerholt (2000) comments specifically on the postural stresses of wind players, which create muscle imbalances and trigger point activity. ‘With forward head posture, musicians will have to exert greater muscular force to elevate the arms to hold the instrument. Wind instrumentalists with forward head posture may have difficulty with their embouchure, and may complain of pain in the temporomandibular region, in the masticatory muscles, or in their respective referred pain zones.’
• Brugger (1980) and others have reported that breathing patterns may be impaired in such instrumentalists, with negative effects on performance.
• String players are obliged to create a prolonged internal rotation of the arms, which allows evolution of myofascial stress in the associated muscles, and consequent arm or shoulder pain.
• Beijani (1993a) evaluated particular restrictions and dysfunctional patterns and found functional spinal deformities in 56% of musicians (mainly thoracic kyphosis and scapular prominence). These included scoliotic changes convex to the left in violinists, cellists and guitarists, with convexities to either side in pianists and harpists (who displayed the highest levels of scoliosis of all those evaluated).
• Beijani (1993b) found that among musicians the most common problems were inflammatory tendons (tendinitis), joint (bursitis) conditions, or disorders involving motor control. The findings of dysfunction in different musician groups are summarized as follows:
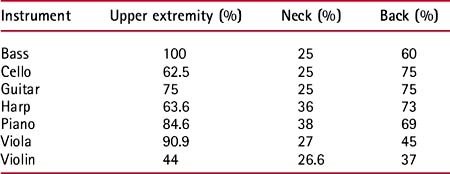
• Ziporyn (1984) noted the following symptoms in a study of 128 string players attending for treatment: stiffness, tension, pain, soreness, spasms or numbness affecting the shoulders, wrist, fingers, neck, jaw and back.
Dommerholt (2000) suggests a broad assessment of dysfunction involving the entire body, very much in line with the themes expressed in this text. ‘Any neuro-muscular reeducation program must consider the involvement of the entire body in playing a musical instrument irrespective of a biomechanical or somatic orientation.’
The assessment should involve examination, evaluation, diagnosis, prognosis and intervention. Those elements of these criteria that are not within the scope of practice of the practitioner should be conducted by appropriately trained and licensed health-care providers.
• Rule out possible underlying medical problems.
• Take history and conduct (or have conducted) systems review and any appropriate tests.
• Take details of instrument played as well as practice and performance schedule and habits.
• Observe the musician standing, seated and walking (without the instrument).
• Look for postural deviations (kyphosis, lordosis, scoliosis, forward head posture, etc.) as well as unbalanced shoulder and pelvic levels, leg length inequalities, foot, ankle, leg misalignments and unusual arm rotation positions.
• Following this, the musician should play the instrument while a visual assessment of postural and functional features is carried out.
• Full assessment of muscular and joint status should then be performed.
• Finally, the musician should be observed carrying the instrument when not performing, enclosed in its case, which is often of substantial weight, as well as other items (music portfolio, mutes, reed trimming equipment) that are often carried at the same time.
Dommerholt, quoted earlier in the section related to sitting, suggests that rehabilitation requires focus on both local and whole muscle dysfunctions and imbalances. ‘Typically, muscle imbalances involve tonic or postural and phasic dynamic muscles’ (see Volume 1, Chapter 2 for discussion of these). He continues: ‘Another important consideration in relation to postural assessment is the presence of myofascial trigger points in the muscles’ and notes that 73% of musicians diagnosed with overuse syndrome were shown in one study (Moran 1992) to have myofascial pain syndrome. Dommerholt insists that: ‘It should be obvious that the presence of forward head posture, muscle imbalances and myofascial trigger points can impair musicians substantially’.
Dental irregularities (such as underbite and overjet) and oral habits (such as tongue thrust and thumb sucking) should be considered when the young musician-to-be is selecting an instrument to learn to play. Since the mouthpiece can create particular strains on dentition, existing dental conditions may influence instrument choices. For instance, a child with an overjet (‘buckteeth’) would be better off choosing an instrument with an externally placed mouthpiece (French horn, trumpet, trombone), which might even mildly assist in correction of the overjet, rather than selecting an internally placed one (clarinet, saxophone) which might negatively influence even professional orthodontic intervention. Likewise, the student with an underbite might benefit from the clarinet rather than the trumpet.
Proper positioning while playing as well as appropriate stretches (prior to and after playing) are best taught as part of the musical curriculum. Given early in the musician’s development, these healthy steps become part of the normal protocol of preparing to play and serve to prevent the development of the pathologies and syndromes discussed in these chapters. Additionally, since better dexterity is likely to be accomplished by these steps, a more skilled and capable musician may be the outcome.
This chapter has shown some of the ways in which the interaction between individuals and the environment of their daily life can powerfully impact the structure and function of the human frame. When the high demands of physical activity, such as that which occurs in sports participation, are overlaid onto these preexisting conditions, and particularly when this is in a sporadic, infrequent manner, injuries are likely to result. This may also be true for professional athletes due to the very frequent repetitions of movements which sports demand of their bodies, as well as the day-to-day habits they encounter outside their sporting activities. The following chapter explores some of the unique demands of sports and some of the dysfunctions that may result.
Alexander F. The use of the self. Downey, California: Centerline Press, 1984.
Barlow W. The Alexander principle. London: The Orion Publishing Group Ltd, 1975.
Barelli P. Neuropulmonary physiology. In: Timmons B., editor. Behavioral and psychological approaches to breathing disorders. New York: Plenum Press, 1994.
Beijani F. Current research in arts medicine. Chicago: Capella Books, 1993.
Beijani F. Occupational disorders of performing artists. In Delisa J., Gans B., Currie M., editors: Rehabilitation medicine, ed 2, Philadelphia: Lippincott, 1993.
Bigos S., Holland J., Webster M. Reliable science about avoiding low back problems at work. New York: Springer-Verlag, 1998.
Birch L., Graven-Nielsen T., Christensen H., et al. Experimental muscle pain modulates muscle activity and work performance differently during high and low precision use of a computer mouse. Eur J Appl Physiol. 2000;83(6):492-498.
Bradley D. Hyperventilation syndrome/breathing pattern disorders. Auckland, New Zealand: Tandem Press, 1998. Kyle Cathie, London, UK. Hunter House, San Francisco, California
Braggins S. Back care: a clinical approach. Edinburgh: Churchill Livingstone, 2000.
Brennan R. The Alexander technique workbook. Shaftsbury, Dorset: Element Books, 1992.
Brugger A. Pseudoradikulare syndrome. Acta Rheumatol. 1960;18:1.
Brugger A. Die Erkrankungen des Bewegungs apparates und seines Nervensystems. Stuttgart: Gustav Fisher Verlag, 1980.
Burke J.P. Whiplash and its effect on the visual system. Grafes Arch Clin Exp Ophthalmol. 1992;230:335-339.
Buskila D., Neumann L. Increased rates of fibromyalgia following cervical spine injury. Arthritis Rheum. 1997;40(3):446-452.
Butler D. Mobilisation of the nervous system. Edinburgh: Churchill Livingstone, 1991.
Buytendijk F. Algemene theorie der menselijke houding in beweging. Utrecht: Het Spectrum, 1964.
Chaitow L. Modern neuromuscular techniques, ed 3. Edinburgh: Churchill Livingstone, 2010.
Chester J.B. Whiplash, postural control and the inner ear. Spine. 1991;16:716-720.
Cottle M. Rhinomanometry. Kansas City, Missouri: American Rhinological Society, 1980.
Cranz G. Alexander technique in the world of design (pt 1). Journal of Bodywork and Movement Therapies. 2000;4(2):90-98.
Cranz G. Alexander technique in the world of design (pt 2). Journal of Bodywork and Movement Therapies. 2000;4(3):155-165.
Davies A., Koenig J., Thach B. Characteristics of upper airway chemoreflex prolonged apnea in human infants. American Review of Respiratory Diseases. 1989;139:688-1673.
Decina L., Kneobel K. Child safety seat misuse patterns in four states. Accid Anal Prev. 1997;29:125-132.
Dischinger P., Ho S., Kerns T. Patterns of injury in frontal collisions with and without airbags. Proceedings of the International IRCOBI Conference on the Biomechanics of Impact. 1996:311-320.
Dommerholt J. Posture. In: Tubiana R., Camadio P., editors. Medical problems of the instrumentalist musician. London: Martin Dunitz, 2000.
Fontana L., Neel S., Claise J., et al. Osteoarthritis of the thumb carpometacarpal joint in women and occupational risk factors: a case-control study. J Hand Surg [Am]. 2007;32(4):459-465.
Foret-Bruno J. Influence of the seat and head rest stiffness on the risk of cervical injuries in rear impact. Proceedings of the 13th ESV Conference, Paris. Washington DC: NHTSA; 1991.
Gustafsson E., Johnson P., Hagberg M. Thumb postures and physical loads during mobile phone use – A comparison of young adults with and without musculoskeletal symptoms. J Electromyogr Kinesiol. 2009. Article in Press
Hannon J. Pillow talk: the use of props to encourage repose. Journal of Bodywork and Movement Therapies. 1999;3(1):55-64.
Hannon J. The physics of Feldenkrais part 2. Journal of Bodywork and Movement Therapies. 2000;4(2):114-122.
Hannon J. Presentation. Journal of Bodywork and Movement Therapies Conference, Dublin. May 2000.
Hannon. Connective tissue perspectives: stillness, salience and the sensibilities of stroma. Journal of Bodywork and Movement Therapies. 2000;4(4):280-284.
Hannon. The physics of Feldenkrais part 3. Journal of Bodywork and Movement Therapies. 2000;4(4):261-272.
Heffner S. McKenzie protocol in cervical spine rehabilitation. In: Murphy D., editor. Conservative management of cervical spine syndromes. New York: McGraw-Hill, 2000.
Hoppenfeld S. Physical examination of the spine and extremities. Norwalk, Connecticut: Appleton and Lange, 1976.
Kapandji A. Anatomy of the spine. In: Tubiana R., Camadio P., editors. Medical problems of the instrumentalist musician. London: Martin Dunitz, 2000.
Kaplan A., Williams G. The tmj book. New York: Pharos Books, 1988.
Karlqvist L., Bernmark E., Ekenvall L., et al. Computer mouse and track-ball operation: Similarities and differences in posture, muscular load and perceived exertion. International Journal of Industrial Ergonomics. 1999;23(3):157-169.
Kendall F., McCreary E., Provance P. Muscles, testing and function, ed 4. Baltimore: Williams and Wilkins, 1993.
Kiesewetter H. Effects of garlic coated tablets in peripheral arterial occlusive disease. J Clin Invest. 1993;71(5):383-386.
Koch M. Soft tissue injury of the cervical spine in rear-end and frontal car collisions. Proceedings of the International IRCOBI Conference on the Biomechanics of Impact, Switzerland. 1995:273-283. September 13–15
Kopell H., Thompson W. Peripheral entrapment neuropathies. Baltimore: Williams and Wilkins, 1963.
Larder D. Neck injury to car occupants using seat belts. Proceedings of the 29th Annual Meeting of the American Association for Automotive Medicine, Washington DC. 1985:153-165.
Lee D. The pelvic girdle, ed 2. Edinburgh: Churchill Livingstone, 1999.
Lewit K. Manipulative therapy in rehabilitation of the motor system. London: Butterworths, 1983.
Lewit K. Manipulative therapy in rehabilitation of the locomotor system. London: Butterworths, 1985.
Lewit K. Manipulative therapy in rehabilitation of the motor system, ed 3. London: Butterworths, 1999.
Liebenson. Advice for the clinician. Journal of Bodywork and Movement Therapies. 1999;3(3):147-148.
Lockett R. Computering and exercise: escaping the aches and pains of computer work. Clearwater, Florida: Rockett Publications, 1999.
Maag U., Dejardins D., Borbeau R. Seat belts and neck injuries. International IRCOBI Conference on the Biomechanics of Impact, Lyon, France. 1990:1-13. September 12–14
MacKinnon S., Dellon A. Surgery of the peripheral nerve. New York: Thieme, 1988.
McIlwraith B. An analysis of the driving position in the modern motor car. British Osteopathic Journal. 1993;11:27-33.
McKenzie. The lumbar spine: mechanical diagnosis and therapy. Waikane, New Zealand: Spinal Publications, 1981.
Meador R. The treatment of shoulder pain and dysfunction in a professional viola player. J Orthop Sports Phys Ther. 1989;11:52-55.
Mennel J.M. Back pain. London: Churchill, 1960.
Mennel J.M. Joint pain. London: Churchill, 1964.
Mitchell G. Autonomic nerve supply to the throat, nose and ear. J Laryngol Otol. 1964;68:495-516.
Moles R. Ending head and neck pain: the T.M.J. connection. Racine, Wisconsin: CGM, 1989.
Moran C. Using myofascial techniques to treat musicians. J Hand Ther. 1992;5:97-101.
Morris A., Thomas P. Neck injuries in the UK cooperative crash injury study. Society for Automotive Engineers, 1996.
Murphy D. Conservative management of cervical spine syndromes. New York: McGraw-Hill, 2000.
Ming Z., Pietikainen S., Hanninen O. Excessive texting in pathophysiology of first carpometacarpal joint arthritis. Pathophysiology. 2006;13(4):269-270.
NHTSA. Child restraint systems safety plan. National Highway Traffic Safety Administration; 2000. www.nhtsa.dot.gov.
Nordhoff L. Cervical trauma following motor vehicle collisions. In: Murphy D., editor. Conservative management of cervical spine syndromes. New York: McGraw-Hill, 2000.
Phelps S., Harris W. Garlic supplementation and lipoprotein oxidation susceptibility. Lipids. 1993;28:475-477.
Pope M. Biomechanics of the lumbar spine. In: Frymoyer J., editor. The adult spine. New York: Raven Press, 1991.
Prior T. Biomechanical foot function: a podiatric perspective. Journal of Bodywork and Movement Therapies. 1999;3(3):169-184.
Rosenthal E. The Alexander technique and how it works. Medical Problems in the Performing Arts. 1987;2:53-57.
Rouhana S. Biomechanics of abdominal trauma. In: Accidental injury: biomechanics and prevention. New York: Springer-Verlag; 1993:391-428.
Rutledge R., Thomason M., Oller D., et al. The spectrum of abdominal injuries associated with the use of seat belts. J Trauma. 1991;31:820-826.
Sachs M., Tombrello S. Car seats safety: buckling up isn’t always enough. Pediatric Basics. 2000;90:11-24.
Schafer R. Clinical biomechanics, ed 2. Baltimore: Williams and Wilkins, 1987.
Simons D., Travell J., Simons L. Myofascial pain and dysfunction: the trigger point manual, vol 1, upper half of body, ed 2. Baltimore: Williams and Wilkins, 1999.
Singer S., Grismaijer S. Dressed to kill: the link between breast cancer and bras. Garden City Park, New York: Avery, 1995.
Taddey J. Musicians and temporomandibular disorders. Cranio. 1992;10:241-244.
Thompson F., Coughlin M. The high price of high-fashion footwear. J Bone Joint Surg Am. 1994;76:1586-1593.
Tikoff G. Diseases of peripheral arteries and veins. In: Stein J., editor. Internal medicine. Boston: Little, Brown, 1983.
Timmons B. Behavioral and psychological approaches to breathing disorders. New York: Plenum Press, 1994.
Travell J., Simons D. Myofascial pain and dysfunction: the trigger point manual, vol 2, the lower extremities. Baltimore: Williams and Wilkins, 1992.
Waddell G. The back pain revolution. Edinburgh: Churchill Livingstone, 1998.
Wahlstrom J., Svensson J., Hagberg M., et al. Differences between work methods and gender in computer mouse use. Scand J Work Environ Health. 2000;26(5):390-397.
Weber K. Crash protection for child passengers: a review of best practice. Ann Arbor, Michigan: University of Michigan Transportation Research Institute, 2000.
Wenberg S., Thomas J. The role of vision in the rehabilitation of the musculoskeletal system. Journal of Bodywork and Movement Therapies. 2000;4(4):242-245.
Wilson A. Are you sitting comfortably? London: Optima, 1994.
Ziporyn T. Pianist’s cramp to stage fright: the medical side of music-making. J Am Med Assoc. 1984;252:985-989.